Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 4
18 - Associations between Adverse Events and Mechanisms of Intensive Care Unit Triage in Hospitalized Children
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 18
Publication Number: 18.3244
Publication Number: 18.3244

Lisa Rickey, MD, MHQS
Pediatric Hospitalist
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Adverse events (AEs) occur frequently in the inpatient setting, especially around escalations of care. Previous studies have demonstrated high rates of AEs associated with unplanned transfers from inpatient units to Intensive Care Units (ICU). In our institution activation of a tiered rapid response team (RRT) facilitates inpatient ICU triage by non-urgent (ICU Eval) or emergent (ICU Stat/Code Blue) mechanisms. We sought to measure rates of adverse events before and after escalations of care, and to assess whether they varied by the urgency level of ICU triage.
Objective: To assess whether the urgency of ICU triage is associated with differences in the risk, severity, or preventability of AEs prior to and immediately following ICU transfer.
Design/Methods: Retrospective study of patients < 18 years admitted to inpatient medical and surgical units from January 2018-December 2019 with unplanned ICU transfers. Patients with RRT activations without transfer were also evaluated for comparison. Primary reviewers performed a focused chart review, informed by a modified GAPPS trigger tool, from admission to RRT activation (pre-transfer), and during the first 48 hours of ICU admission (post-transfer). All suspected AEs identified on primary review underwent secondary review by two independent physicians, who made final judgments regarding case classification (91% agreement, K=0.63), severity level, and preventability.
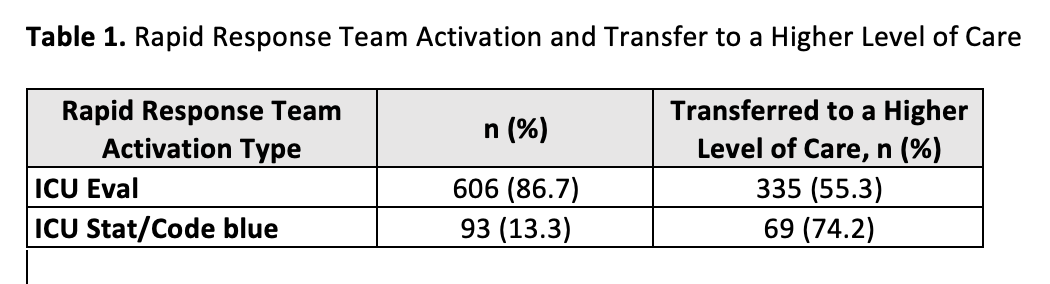
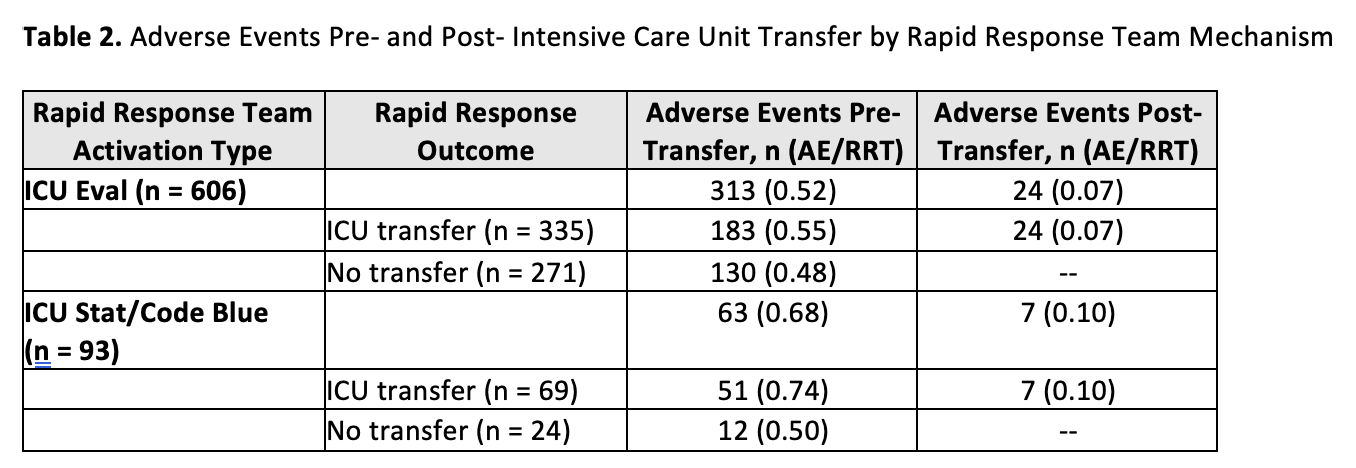
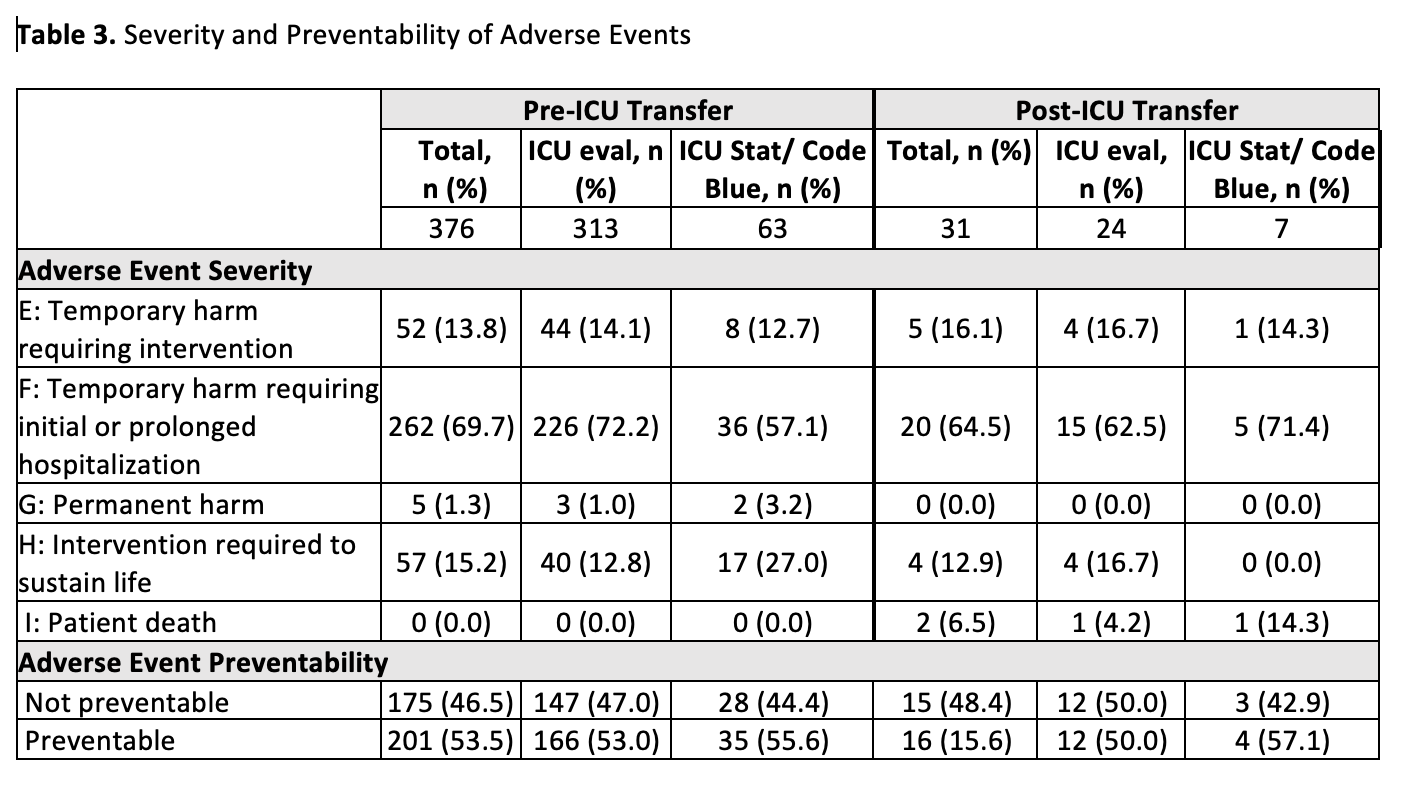
Results: Our cohort includes 699 RRT activations triaged as ICU Eval (86.7%, n=606) or ICU Stat/Code Blue (13.3%, n=93) and ICU transfer was common in this population (55.3% and 74.2%, respectively). AEs were 31% more common among ICU Stat/Code Blue v ICU Eval activations (0.68 v 0.52 AE/RRT) prior to ICU transfer. Most AEs resulted in temporary harm requiring initial or prolonged hospitalization (NCC-MERP Level F, 69.7%) or interventions required to sustain life (H, 15.2%) and 53.5% were preventable. In the post-transfer cohort, AEs occurred less frequently (n=31) and rates were slightly higher among patients transferred via ICU Stat/Code Blue v ICU Eval mechanisms (0.10 v 0.07 AE/RRT). The majority of AEs were moderate in severity (E, 16.1% and F, 64.5%) and similar between transfer mechanisms (p=0.66).
Conclusion(s): We identified high rates of AEs among patients requiring ICU triage and transfer, especially among those transferred by emergent mechanisms. We have also demonstrated that activation of a rapid response team and/or transfer to higher level of care is a high yield trigger for AE detection.