Hospital Medicine
Session: Hospital Medicine 3
341 - Nurse Education and Perceived Comfort and Effectiveness on Working with Medical Interpreters
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 341
Publication Number: 341.136
Publication Number: 341.136

Devin T. VanWanzeele, DO (she/her/hers)
PHM Fellow
University of Nebraska College of Medicine
Omaha, Nebraska, United States
Presenting Author(s)
Background: In a 2019 census bureau survey, 22% of families in the United States spoke a language other than English in their homes. Within the healthcare system, these language barriers have led to poor quality of care and adverse events. Per review of the literature, there is little regarding if health care providers, outside of medical students, receive education on working with medical interpreters
Objective: Complete a cross-sectional survey of pediatric nurses at a free-standing tertiary care children’s hospital regarding prior training, comfort, and self-reported effectiveness related to working with medical interpreters.
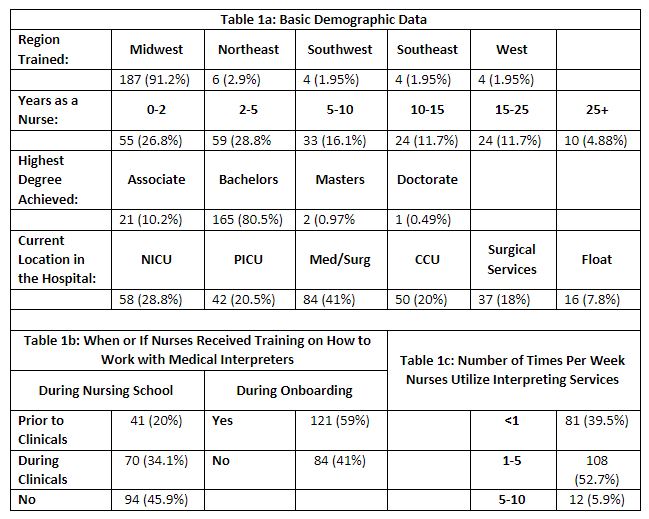
Design/Methods: At a Midwestern, free-standing tertiary care children’s hospital, bedside nurses from multiple units were approached for a voluntary twelve question survey which collected basic demographic data, prior interpreter education, and perceived comfort/effectiveness utilizing interpreting services utilizing a Likert scale.
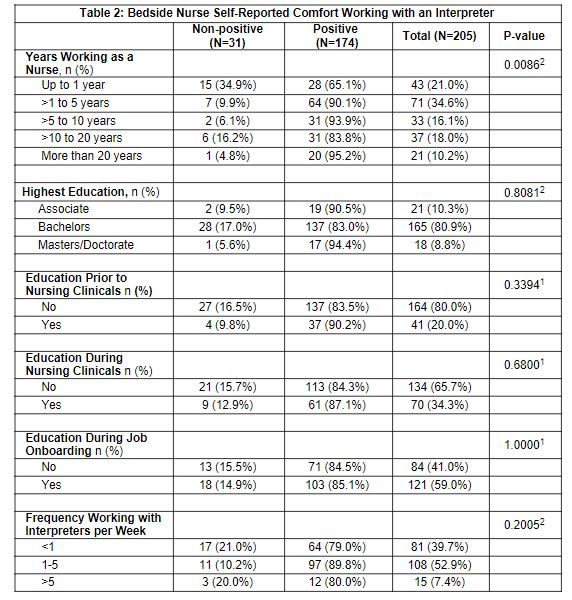
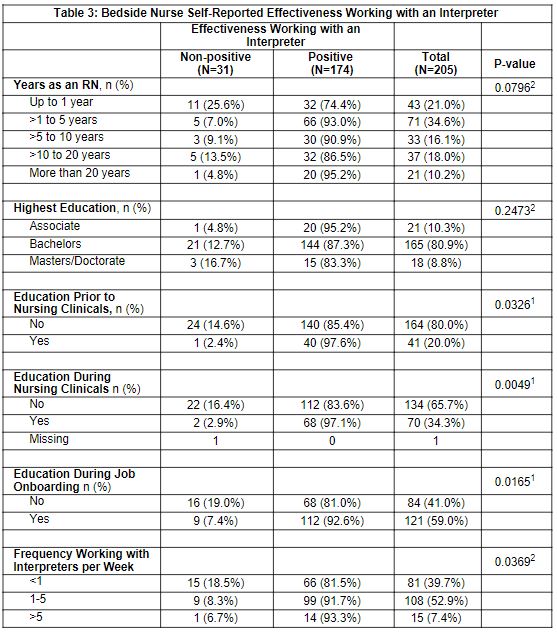
For statistical analysis, descriptive outcomes were calculated. For comparison of self-confidence and effectiveness, Likert responses were grouped as positive (strongly agree or agree) and non-positive (neutral, disagree, or strongly disagree). Groups were compared using Fisher’s exact tests or Cochran-Armitage trend tests.
Results: 205 bedside nurses completed the survey, accounting for 57% of the population. Table 1 provides the demographic information and reported education exposure of the cohort. The nurses with positive self-reported comfort demonstrated a positive association with the number of years worked (p = 0.008)(table 2). There was no statistical association between prior training on using an interpreter and reported comfort level (p= 0.33). There was a statistically significant association between perceived effectiveness using an interpreting service and both prior training on using an interpreter (p= 0.03) and how frequently a nurse utilized interpreting services (p= 0.0369)(table 3).
Conclusion(s): Despite bedside nurses commonly utilizing interpreter services, more than 40% have not received training during nursing school or hospital onboarding. More than one third of nurses in the first year of their career do not report comfort when utilizing interpreting services. However, when nurses received education or utilized the interpreters more frequently, there was a positive perceived effectiveness in communication. This study demonstrates the limited education provided to nurses and the significant lack of confidence a significant group has in working with medical interpreters.