Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 8
315 - Food insecurity and poorer maternal health among mothers with hospitalized infants
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 315
Publication Number: 315.1789
Publication Number: 315.1789
Pyone David, MD (she/her/hers)
Neonatology Fellow
Comer Children's Hospital at University of Chicago Medical Center
Chicago, Illinois, United States
Presenting Author(s)
Background: Food insecurity (FI) rates among households with children are higher than households without children (12.5% vs 9.4%). Increasingly, children's hospitals are integrating social with medical care by assessing families for and addressing FI. CommunityRx-Hunger (CRx-H) is a hospital-based intervention in a predominantly African American/Black community providing support to alleviate FI and other health-related social risks for families with hospitalized children.
Objective: To assess the relationship between FI and physical and mental health among mothers with a hospitalized infant < 1 year of age between 2021-2022.
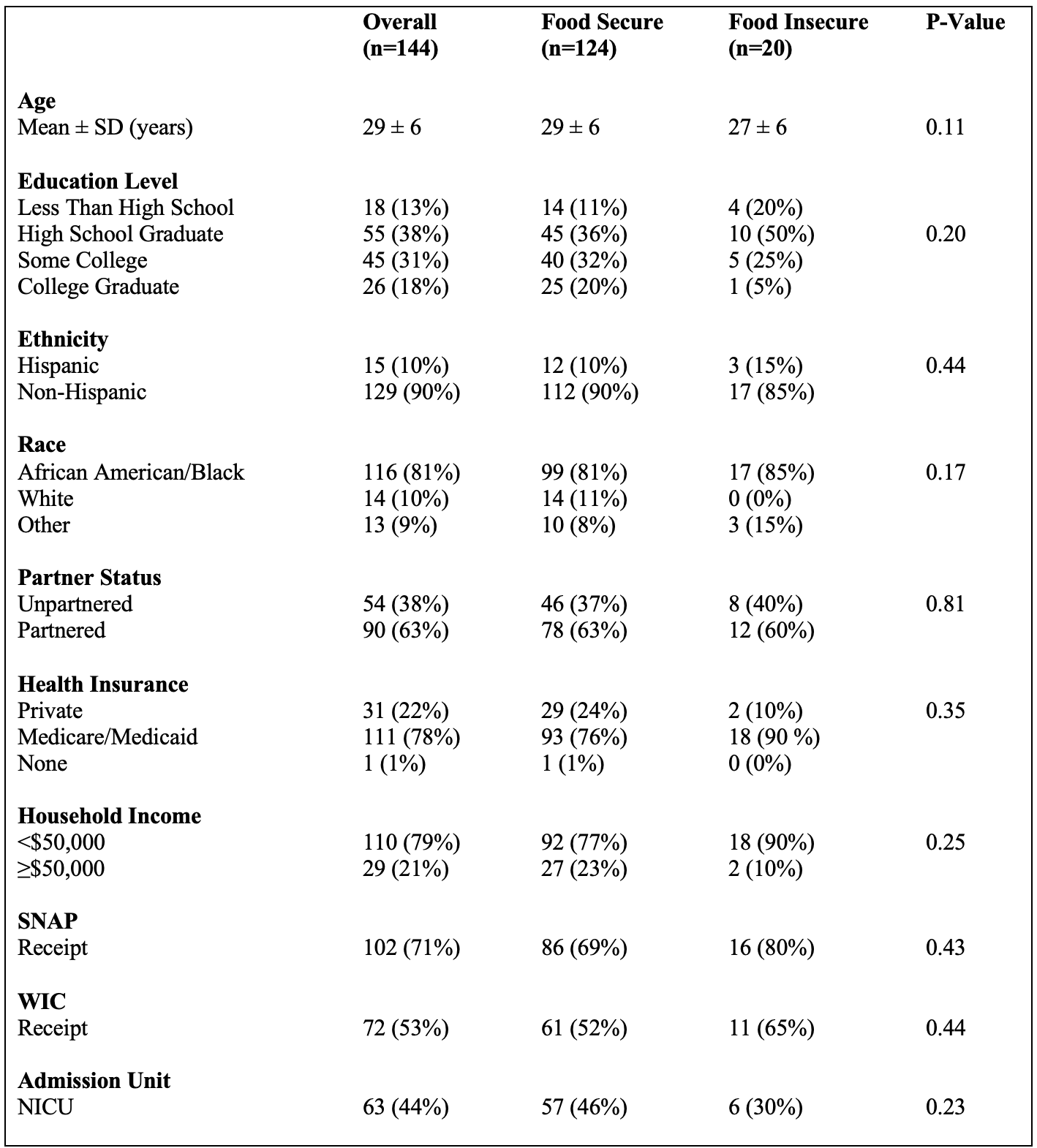
Design/Methods: Baseline data from 144 CRx-H participants at a Chicago urban academic medical center were descriptively analyzed comparing mothers from food secure (FS) and FI households. FS status in the prior 30 days was measured using the U.S. Household Food Security Survey (FS < 3 and FI ≥3). Other measures included: sociodemographic characteristics, self-reported knowledge and use of food assistance supports (including Supplemental Nutrition Assistance Program [SNAP] and Women, Infants, and Children [WIC]) and self-reported maternal physical and mental health (PROMIS Global Health Scale, higher scores representing better health). Fisher’s exact test was used for categorical variables and two-sample t-tests were used for continuous variables.
Results: Fourteen percent of 144 mothers were food insecure (n=20). Sociodemographic characteristics, neonatal intensive care unit admission rates, knowledge of community-based food supports and use of SNAP and WIC were similar among FI and FS groups (Tables 1, 2). Among participants with knowledge of each food support type, those with FI reported higher use of free food (p=0.04) and free meal (p=0.002, Table 2) resources. Mothers experiencing FI had lower self-reported physical (p < 0.001) and mental health (p < 0.001) compared to those who were food secure (Figure 1).
Conclusion(s): One in eight mothers with a hospitalized infant was food insecure, which was associated with poorer physical and mental health. SNAP/WIC rates among women from FI households may indicate some under-utilization, given similar sociodemographic characteristics and higher use of other food support services than FS mothers. The inpatient pediatric encounter may present an opportunity to increase SNAP/WIC and other food support use.

.png)
