Adolescent Medicine
Session: Adolescent Medicine 3
170 - Development and pilot testing of an adolescent HIV and STI prevention intervention
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 170
Publication Number: 170.142
Publication Number: 170.142

Sarah Wood, MD, MS (she/her/hers)
Assistant Professor
Perelman School of Medicine at the University of Pennsylvania
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Adolescents are at disproportionate risk of HIV and sexually transmitted infections (STIs), suggesting a need for novel prevention interventions.
Objective: We aimed to describe intervention development and pilot acceptability, fidelity, and retention for a novel primary care-based STI and HIV prevention intervention.
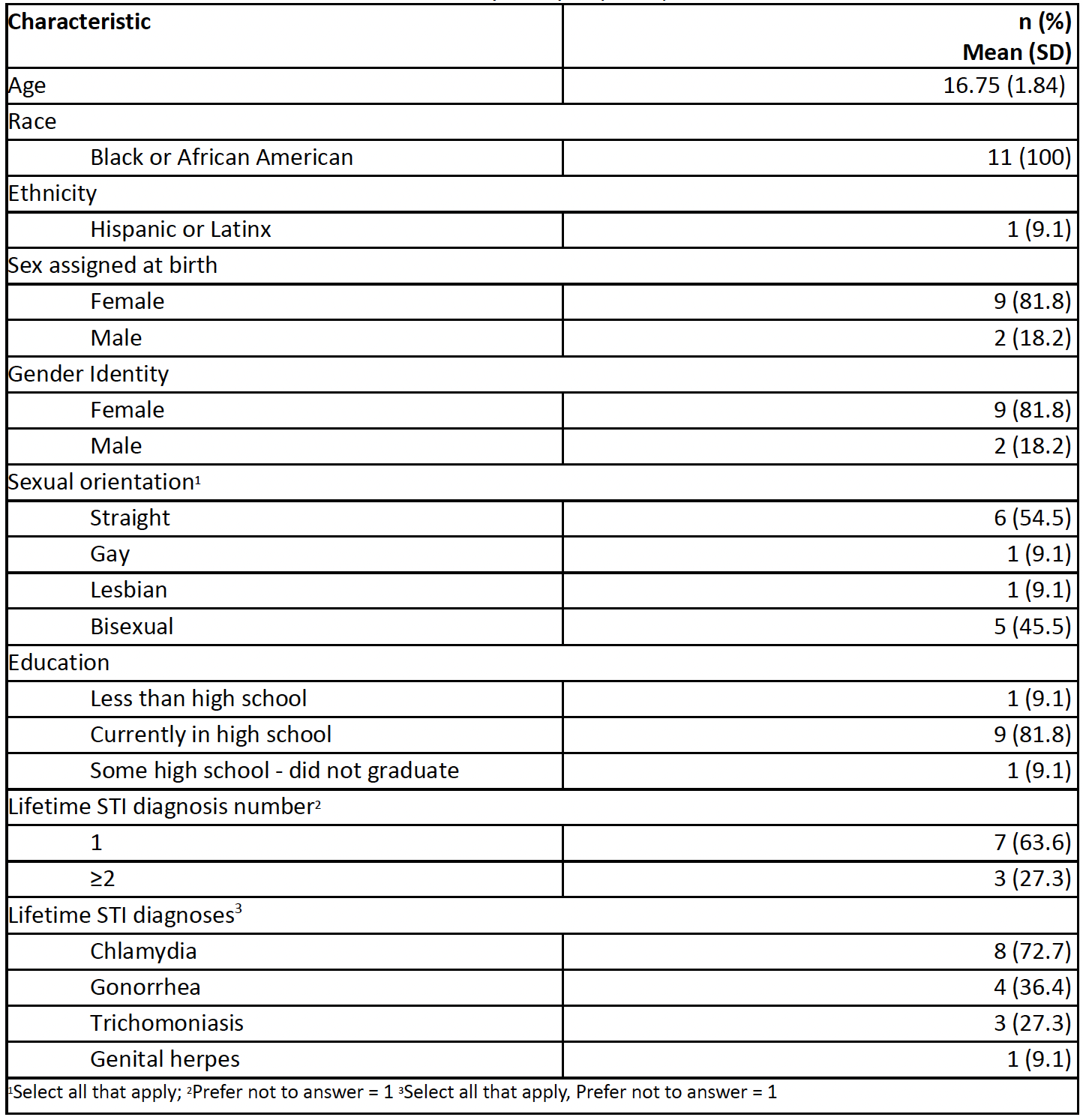
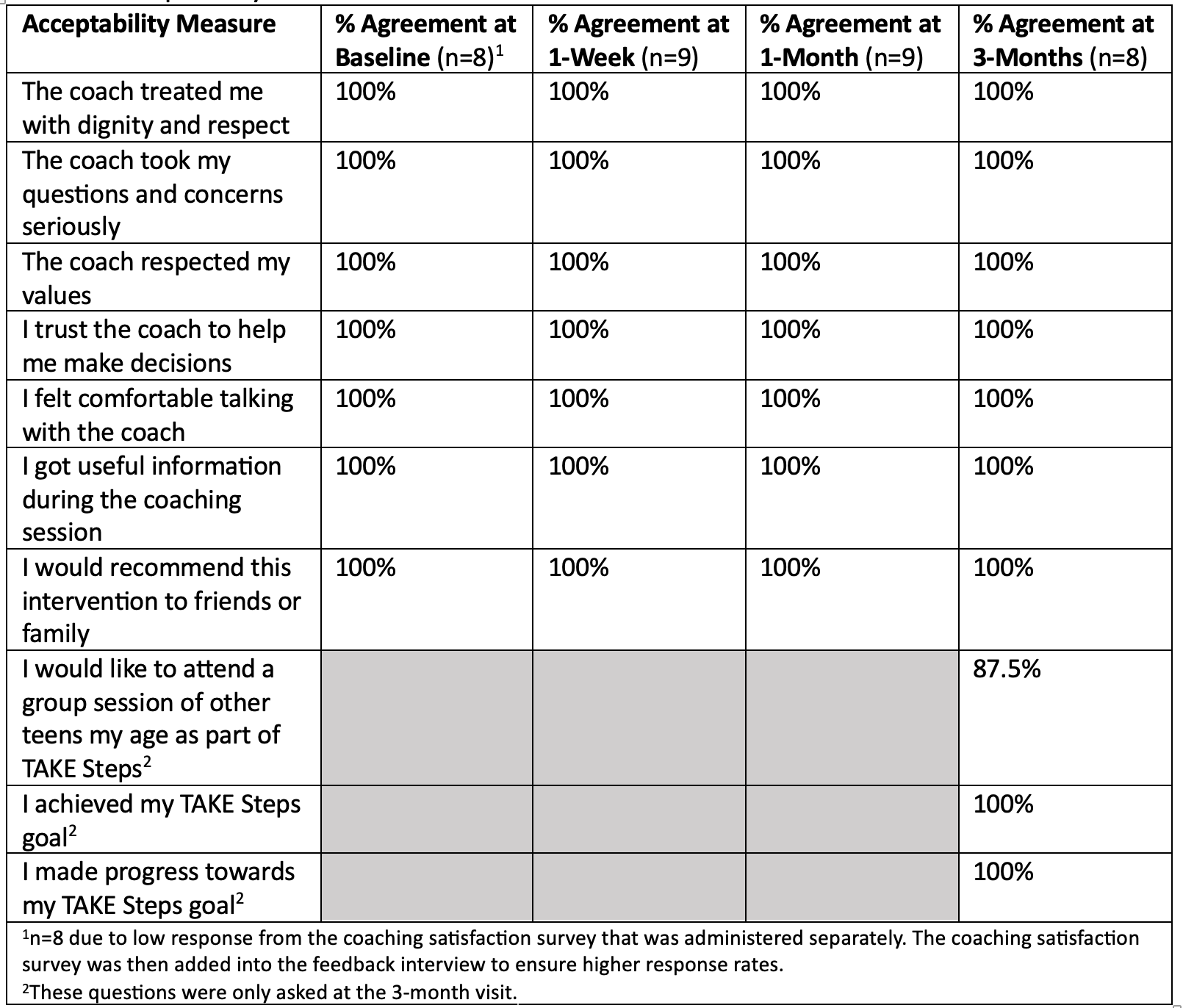
Design/Methods: Adolescents aged 13-19 years with gonorrhea, chlamydia, trichomonas, or syphilis at two urban primary care practices enrolled in a pilot of the newly-developed TAKE (Treat, Act, Know, Engage) Steps intervention. In this 4-session intervention, trained health coaches used motivational interviewing (MI) to increase activation for prevention behavior and support teens in identifying prevention goals (Figure 1), and included adapted elements from Interpersonal Psychotherapy Adolescent Skills Teaching (IPT-AST) to strengthen their interpersonal communication skills. We measured acceptability with a 7-item scale and retention as the proportion of youth attending intervention sessions. We measured fidelity to MI using the 1-Pass system and fidelity to IPT-AST with scale items assessing quality and content of IPT-AST skills. Our analysis included data from all consented adolescents who completed at least one TAKE Steps session (N=11; 84.6%).
Results: Most participants were Black cisgender females (Table 1). Approximately half (54.5%) identified as heterosexual. At baseline, 18% used condoms consistently, 0% were aware of PrEP, 54.5% had completed STI partner notification, and 18.2% had been HIV tested. All 4 sessions were completed by 72% of participants, and 81% and 18% completed 2 and 1 session(s), respectively. All sessions scored at or above the 1-Pass competency thresholds (mean score 5.78, SD 0.29). Mean IPT-AST fidelity ratings were 89% and 91% for content and quality items across sessions, respectively. TAKE Steps was highly acceptable (Table 2). Participant feedback included adding group sessions, increasing mental health elements, and shortening session lengths.
Conclusion(s): In a small-scale pilot, the TAKE Steps intervention was acceptable to adolescents with recent STI and most youth were retained in all intervention sessions. Fidelity to IPT-AST and MI met our pre-defined thresholds. To address participant feedback, we added IPT-AST elements to the one-week session to increase mental health content. A randomized controlled trial of the final intervention is ongoing.