Medical Education
Session: Medical Education 2
530 - Know What You Don't Know: A Survey Based Needs Assessment of Pediatric Nephrology to Inform Establishment of National Fellowship Curriculum
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 530
Publication Number: 530.146
Publication Number: 530.146

Laurel Willig, MD, MS (she/her/hers)
Pediatric Nephrology, Associate Professor
Children’s Mercy Kansas City
Kansas City, Missouri, United States
Presenting Author(s)
Background: There are currently 43 certified US pediatric nephrology fellowship programs (PNFP) with 102 applicants matching into PNFP in the past three years. Given that most institution have a small fellowship program, small number of core faculty providing educational opportunities and variable ancillary support, the American Society of Pediatric Nephrology (ASPN) committee of program directors conducted an educational needs assessment (NA).
Objective: Our aim was to assess interest in a national pediatric nephrology (PN) fellowship curriculum, define educational modalities deemed most useful and identify topic areas of interest.
Design/Methods: A survey-based NA was administered to PN fellows and program and associate program directors (PD/APD) belonging to ASPN from May 2023-Oct 2023. Fellows (n=19) and PD/APD (n=20) completed the survey. All participants were surveyed on general demographics and their current educational programming, including currently utilized educational methods, and incorporation of diversity, equity, and inclusion (DEI) into core curriculum. They rated their overall interest in a national curriculum, the most useful educational platform, and prioritized nephrology topics for a national curriculum. Fellows rated their current knowledge in core nephrology areas.
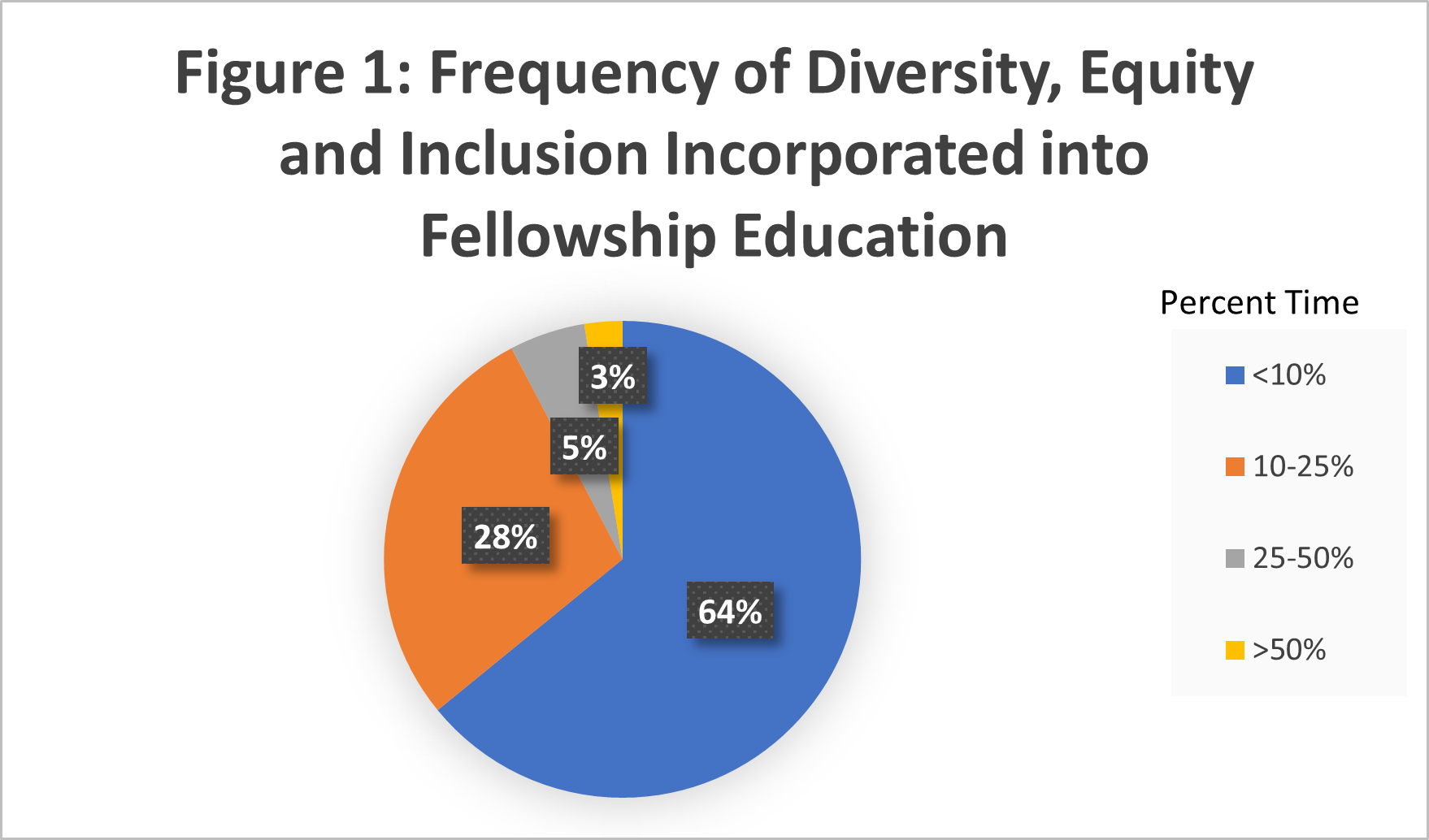
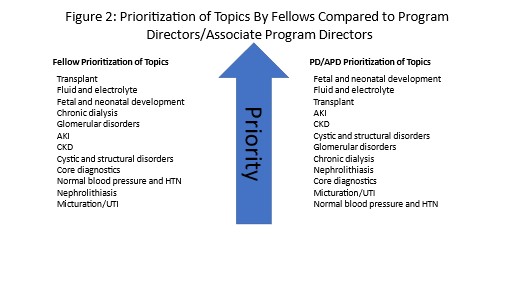
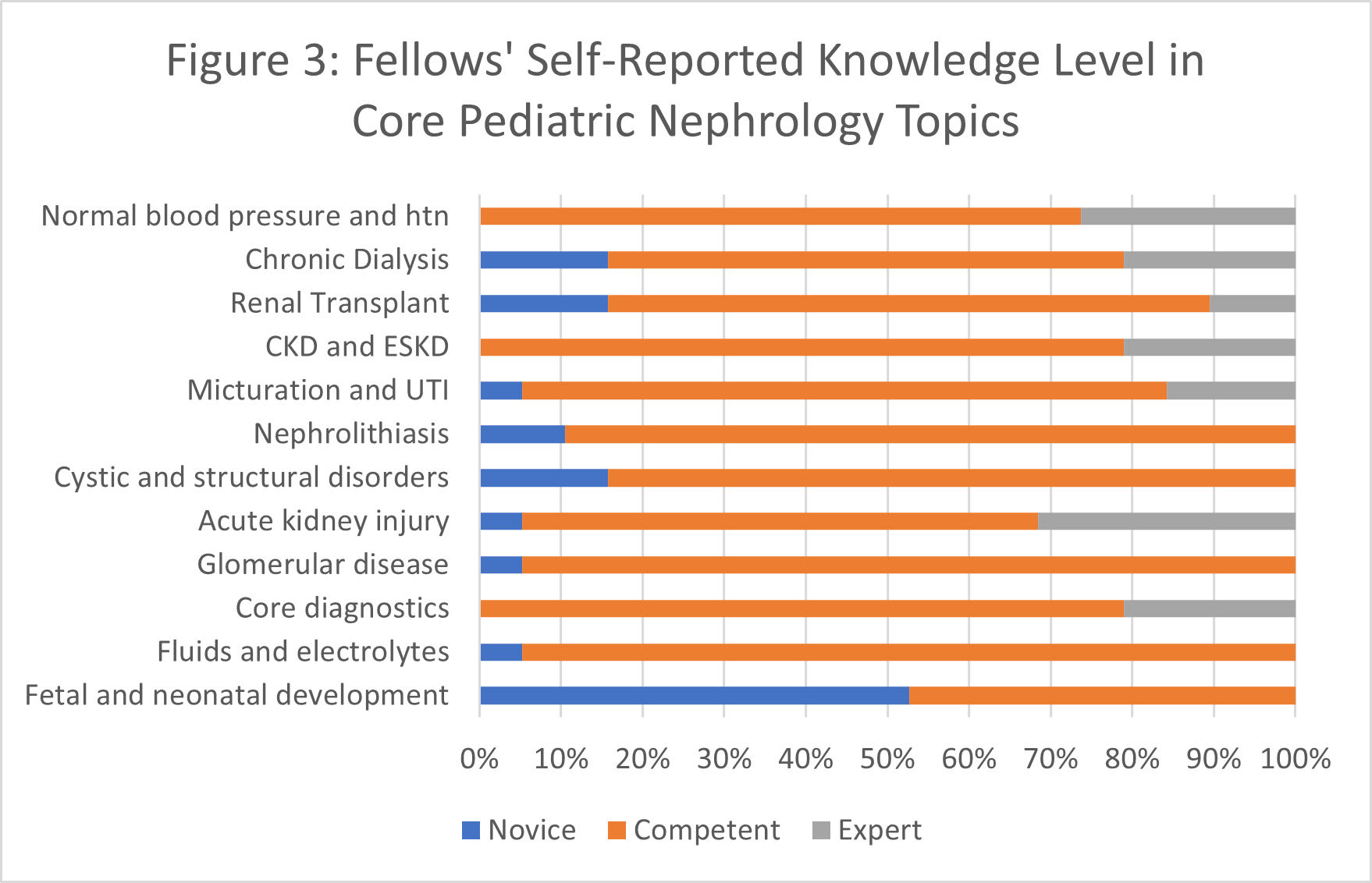
Results: Most utilized current teaching methods were formal lectures, small group discussions like journal clubs, and case-based learning (>90% reporting use sometimes or often) Simulation and flipped classroom techniques were least utilized (>50% reporting use never or rarely). Most participants reported that DEI information was incorporated into lectures < 10% of the time (Fig 1). On scale from 0-100, study participants rated their interest in national curriculum highly (Fellow median=80%, PD/APD= median 85%). Among fellows, 79% felt that a mobile friendly interactive case-based curriculum would be most or somewhat useful, followed by lecture series (63%) and flipped classroom modules (61%). PD/APD also ranked a mobile friendly curriculum most useful. Fellows and PD/APD rank fetal/neonatal kidney development, transplant, and fluid and electrolytes as highest priorities (Fig 2) reflecting the fellows’ ratings of their knowledge base (Fig 3).
Conclusion(s): Most participants felt a national curriculum would be useful. Given the mixed responses to most useful format, a multipronged approach that includes mobile friendly case-based modules and national lecture series would be most effective. The national curriculum should require inclusion of DEI principles and highlight underrepresented groups in biomedical literature.