Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 5
266 - Association of Insurance Status and Individual-level Social Risk Factors with Antihypertensive Medication Prescription and Dietician Referral in Youth with Hypertension Disorders at Baseline
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 266
Publication Number: 266.1564
Publication Number: 266.1564

Estefania G. Narvaez, BS (she/her/hers)
Incoming Medical Student
Atrium Health Wake Forest Baptist
Waxhaw, North Carolina, United States
Presenting Author(s)
Background: Inadequate hypertension (HTN) management in youth is a major concern, contributing to early-life health disparities. Addressing social determinants of health (SDOH), encompassing birth, residence, work, and growth circumstances, is crucial. This includes modifiable and non-modifiable social risk factors, such as healthcare access and affordability.
Objective: Examine if youth referred for HTN with government-sponsored insurance or social risk factors experience differences in pharmacological treatment prescriptions and dietician referrals at baseline.
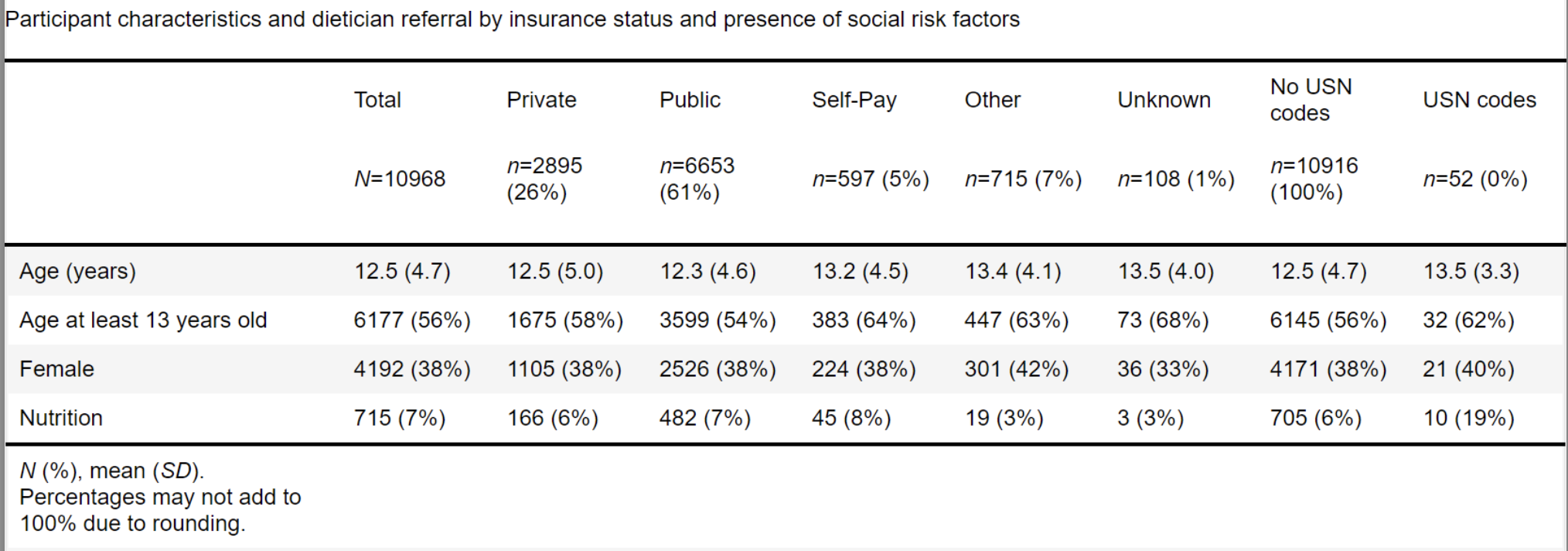
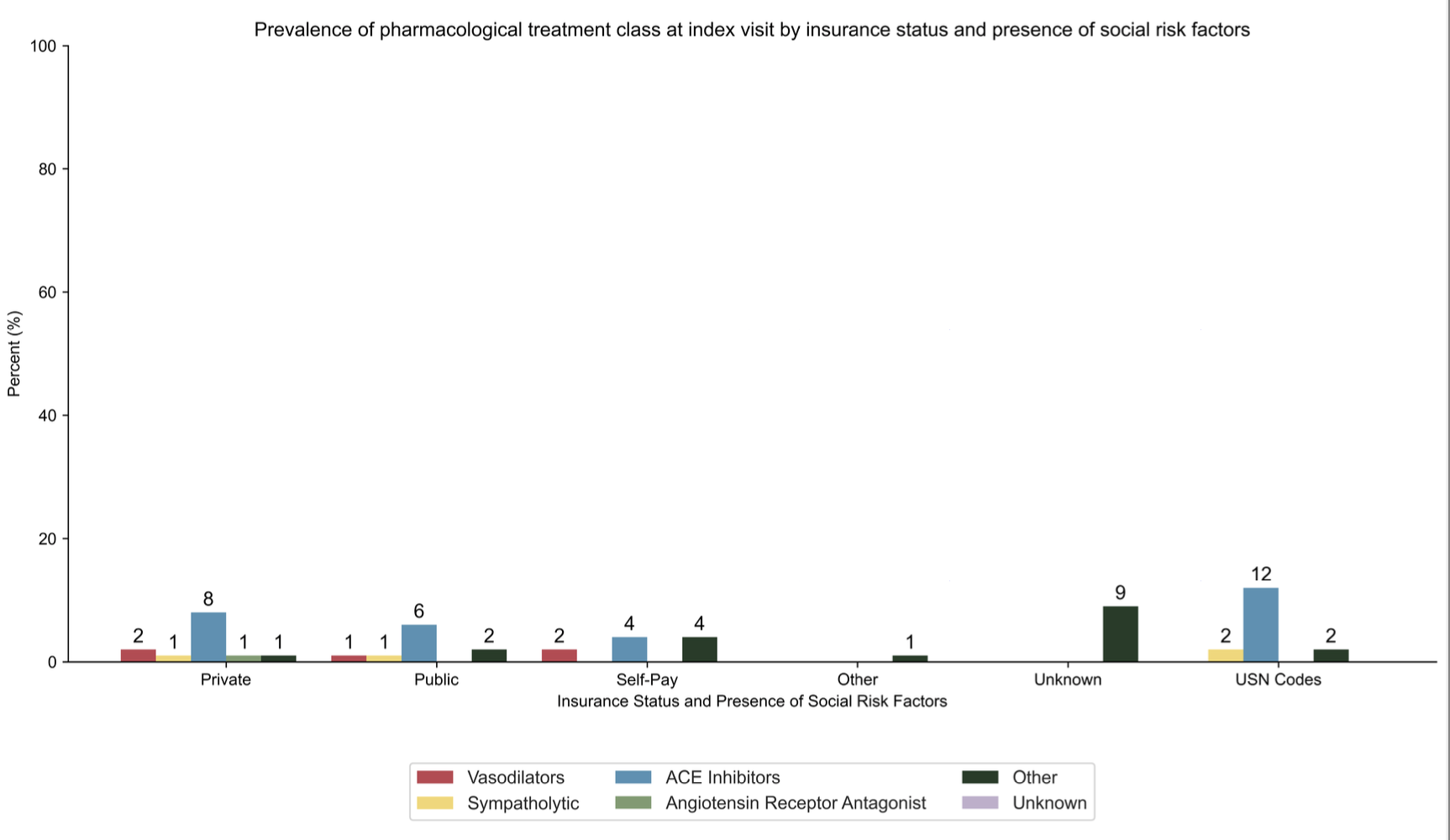
Design/Methods: Cross-sectional analysis of baseline data from the Study of the Epidemiology of Pediatric Hypertension (SUPERHERO), a multisite retrospective Registry of electronic health record data. Inclusion criteria were initial visit for HTN disorder (identified by ICD-10 code) between 1/1/2015 and 12/31/2022 and age < 19 years. Exclusion criteria were ICD-10 code-identified kidney failure on dialysis, kidney transplant, or pregnancy. Our exposures were insurance status and presence of at least one ICD-10 code for a social risk factor, and our outcomes were orders placed for antihypertensive medication prescription and referral to a dietician or weight management clinic. We used generalized linear models.
Results: Of 10,968 participants with mean age 12.5 years, 38% were female, and 61% had government-sponsored insurance. Youth with government-sponsored insurance had a higher likelihood of nutritionist referral (RR 1.3, 95% CL 1.06 to 1.59). No significant associations were found between insurance status and antihypertensive medication prescription or weight clinic referral. Individual-level social risk was associated with increased antihypertensive medication prescription (RR 2.79, 95% CL 1.36 to 5.6) and nutrition referral (RR 3.91, 95% CL 2.09 to 7.31), but not weight clinic referral. ACE inhibitors were the most common initial antihypertensive medication class, and Z59 (housing and economic issues) was the most prevalent social risk factor.
Conclusion(s): Significant differences were found in nutritionist referrals by insurance status, while individual-level social risk factors relate to antihypertensive medication and nutrition referrals. This emphasizes the need to address the social context for youth with HTN, encouraging community collaborations to reduce health disparities. Further analysis should explore the long-term cardiovascular impact of these risk factors to inform targeted interventions.