Medical Education
Session: Medical Education 5
417 - Virtual Essential Newborn Care simulations for skills maintenance in essential newborn care – the Virtual ENC Study
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 417
Publication Number: 417.1556
Publication Number: 417.1556
.jpg)
Rachel Umoren, MBBCH, MS
Associate Professor of Pediatrics
University of Washington
Seattle, Washington, United States
Presenting Author(s)
Background: A child’s risk of death is highest during the first 28 days of life. Up to one-half of these deaths occur on the first day, and three quarters in the first week. This makes the first week of life a critical period for targeted interventions in essential newborn care (ENC) that improve newborn outcomes. Training healthcare professionals in these interventions is essential for efficacy. Computer-based virtual simulations (VS) use established technological and artificial intelligence features to meet the training needs for healthcare professionals.
Objective: To determine the educational efficacy of virtual essential newborn care (vENC) simulations on ENC knowledge and skills retention in health professionals and the optimal frequency of use.
Design/Methods: From Dec 2022-Jun 2023, in-service healthcare workers who provide newborn care participated in a controlled study. Participants had a 2-day in-person training with WHO ENC1 and ENC2 materials. Pre- and immediate post-training evaluations were conducted, before participants were given access to vENC simulation modules on study-specific phones. At the end of study period, a 6-month follow-up evaluation on standardized assessments: ENC1 and ENC2 knowledge checks, bag and mask ventilation skills (BMV), and case scenarios (ENC1 CS A and B, ENC2 CS A and B). Study facilitators used checklists and an advanced manikin [Neonatalie Live, Laerdal] to compare performance across three timepoints—pre-course, immediate post-course (pre-vENC refresher training), and 6-month follow up (post-vENC refresher training) using the Wilcoxon signed-rank test.
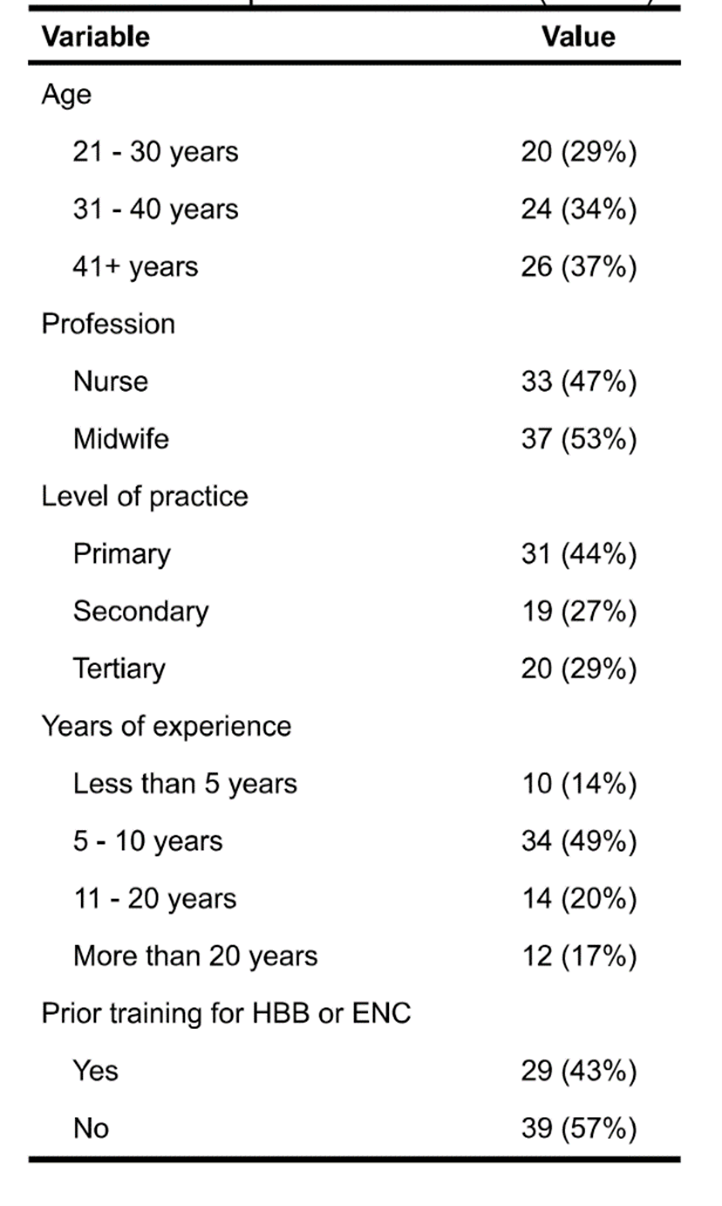
Results: A total of 70 nurses and midwives from 23 Nigeria health facilities (14 primary, 7 secondary and 2 tertiary) participated. See Table 1. 56% reported using vENC at least weekly and 77% at least monthly. Synced data showed, a total of 496 simulation scenarios were completed over 3-4 months by 52 participants, with a total of 39,339 different actions. Scores of all skills assessments improved from before and immediately after the ENC course (p < 0.001). The BMV (p = 0.037), both CSA (p < 0.008) and both CSB scores (p < 0.009) improved between the immediate and 6-month post-course assessments (p < 0.05). Figure 1. Most participants were likely or very likely to report that vENC provided valuable practice (n.51, 85%) and to recommend vENC to a colleague (n.47, 85%).
Conclusion(s): vENC simulations support health professional skills in essential newborn care. Most health professionals tended to use vENC at least monthly.
.png)
