Hospital Medicine
Session: Hospital Medicine 5
148 - Clinician Survey about Antibiotic Prescribing for Children without Definitive Radiographic Pneumonia
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 148
Publication Number: 148.1569
Publication Number: 148.1569

Jillian Cotter, MD, MSCS
Pediatric Hospitalist
University of Colorado / Children's Hospital Colorado
Aurora, Colorado, United States
Presenting Author(s)
Background: While children without definitive evidence of pneumonia on chest radiograph (CXR) are less likely to have bacterial community acquired pneumonia (CAP), many still receive antibiotics.
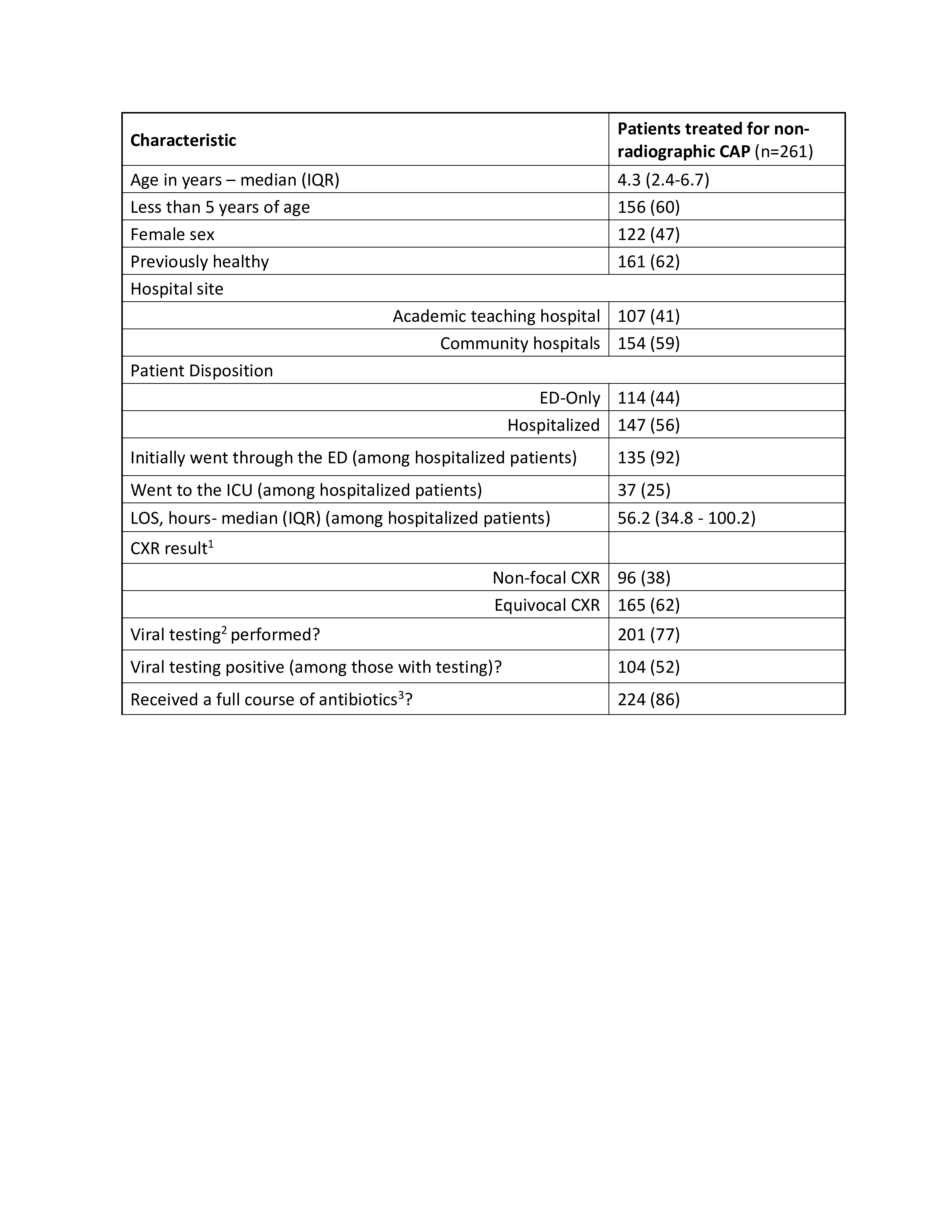
Objective: We aimed 1) to evaluate the proportion of patients treated for bacterial CAP who had non-radiographic CAP (defined as equivocal or non-focal CXR, Table 1), and 2) to understand clinician certainty and factors that influenced their decisions to prescribe antibiotics for children with non-radiographic CAP.
Design/Methods: This was a cross-sectional study of children who received antibiotics for pneumonia and were discharged from the emergency department (ED) or hospitalized at four affiliated children’s hospitals from 5/5/22-11/8/22. Electronic surveys, designed to understand near real-time decision making, were sent to all ED and inpatient clinicians who prescribed antibiotics to patients with non-radiographic CAP in the preceding 48 hours. Additional patient-level data were manually extracted from the electronic medical record.
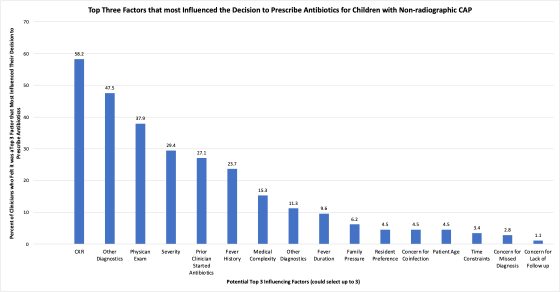
Results: Among 874 patients treated for CAP, 30% (n=261) had non-radiographic CAP (11% non-focal and 19% equivocal CXRs). The proportion with non-radiographic CAP was higher in the ED-only cohort vs. hospitalized cohort (36% vs 26%, p=.002) and at the community sites vs. the academic site (59% vs. 25%, p=.002). Among children with non-radiographic CAP, 60% were < 5 years of age and 86% received a full antibiotic course (Table 1). Among 177 completed surveys (response rate 53%) by clinicians who prescribed antibiotics for children with non-radiographic CAP, 60% were very or mostly certain about the diagnosis. The top three clinician-identified factors that most influenced antibiotic prescribing for children with non-radiographic CAP were CXR findings, other diagnostics (e.g., labs, respiratory testing), and physical exam findings (Figure 1). Clinicians who treated patients with non-focal CXRs identified CXR results as a top three influencing factor 47% of the time. Clinicians who treated patients who were started on antibiotics by a prior clinician (n=82) felt that the prior decision strongly or somewhat strongly influenced their decision to continue antibiotics in 93% of cases.
Conclusion(s): Nearly a third of children who were treated for bacterial CAP had non-radiographic CAP. This suggests that non-radiographic CAP is an important target for antibiotic stewardship. Targeted clinician education regarding CXR interpretation and antibiotic prescribing momentum may help reduce antibiotic overuse.