Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 5
279 - Understanding oral health care utilization in an under-resourced community in Washington DC
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 279
Publication Number: 279.1563
Publication Number: 279.1563

Jessica Weisz, MD
Assistant Professor
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background: Tooth decay, the most common chronic disease in U.S. children, disproportionally affects under-resourced communities leading to poor long-term health outcomes. Since the most recent DC data showed that only 38.5% of Medicaid patients aged 1-20 received preventative dental care, a Community Dental Health Coordinator (CDHC) role was implemented to understand the care gap.
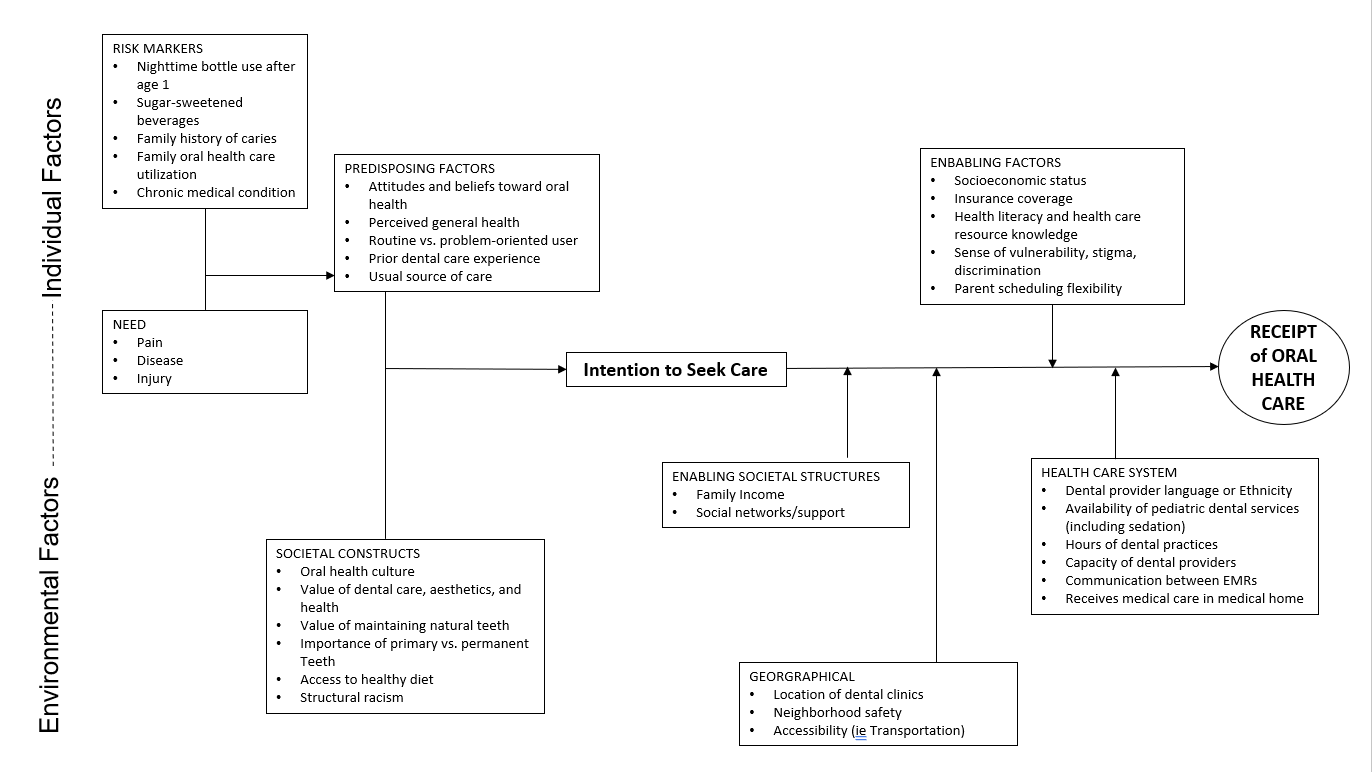
Objective: To describe the individual and environmental factors that impact preventative oral health access in a under-resourced area of Washington DC and analyze rates of preventative dental care between patients of the academic practices’ medical home compared to others.
Design/Methods: Through use of CDHC’s oral access screening and facilitator-led focus groups, factors that impact oral health care utilization were identified. In partnership with the Medicaid agency for Washington DC, rates of patients with preventative oral health care with Medicaid insurance were compared between the academic practices and other children living the same community over a 5-year period.
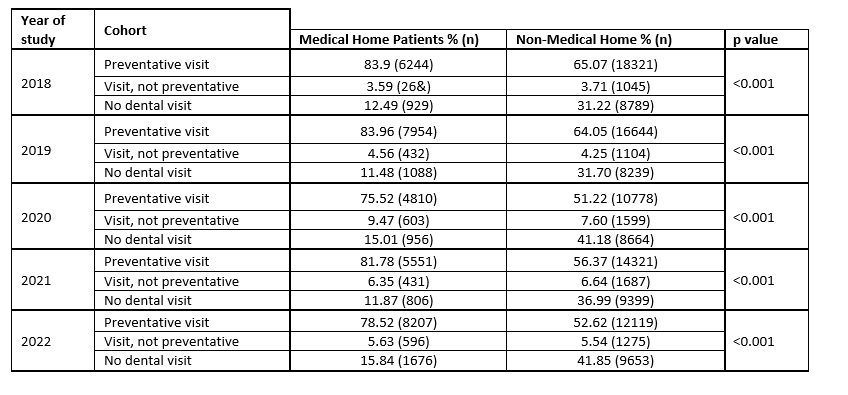
Results: CDHC’s screenings and qualitative focus groups endorsed high rates of dental awareness and utilization. However, parents identified barriers to access included low capacity of existing dental practices (appointments too far in the future) and low flexibility for appointments outside of traditional work hours [Figure 1]. Despite barriers, analysis of Medicaid billing data from 2018 – 2023 showed preventative care among the academic medical home’s patients was higher overall (p < 0.001) before, during, and after the COVID-19 pandemic [Table 1].
Conclusion(s): Rates of preventative care are higher than previously published reports and much higher at the medical homes at our institution than expected. The data suggests that participation in a medical home, with or without co-located dental services, is key to high dental utilization among demographically similar patients. The reason for the difference in utilization rates need to be further evaluated.