Hospital Medicine
Session: Hospital Medicine 5
156 - Nasogastric Hydration Utilization in Bronchiolitis, an EMO Sub-study
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 156
Publication Number: 156.1562
Publication Number: 156.1562

Michael J. Tchou, MD, MSc (he/him/his)
Assistant Professor
University of Colorado-Anschutz and Children's Hospital of Colorado
Aurora, Colorado, United States
Presenting Author(s)
Background: Nasogastric (NG) fluid replacement exists as a safe, effective, and nutritionally beneficial hydration option for pediatric inpatients with bronchiolitis. However, data on the utilization of NG hydration in bronchiolitis across institutions is lacking.
Objective: To describe NG hydration use in bronchiolitis across institutions and its association with clinical factors.
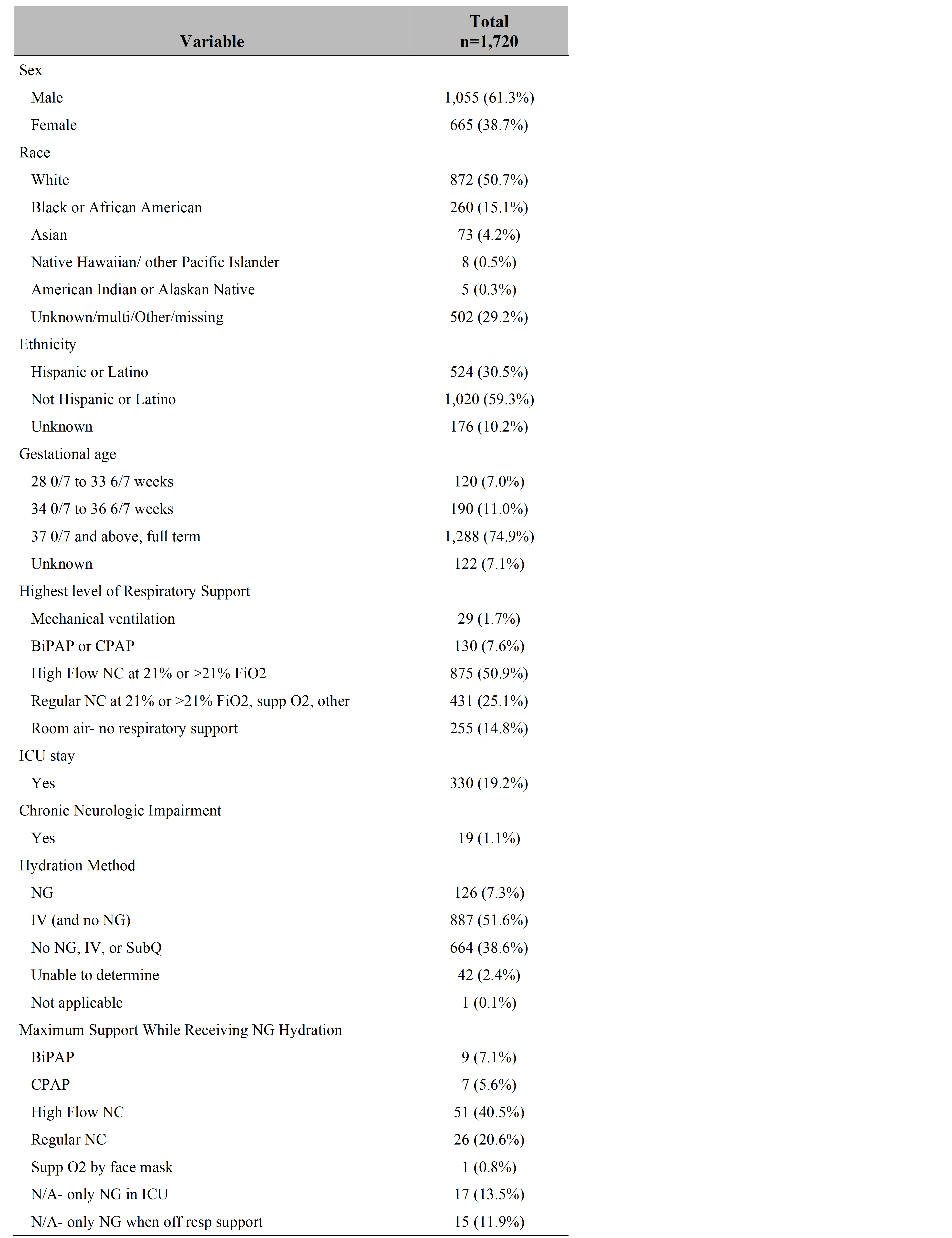
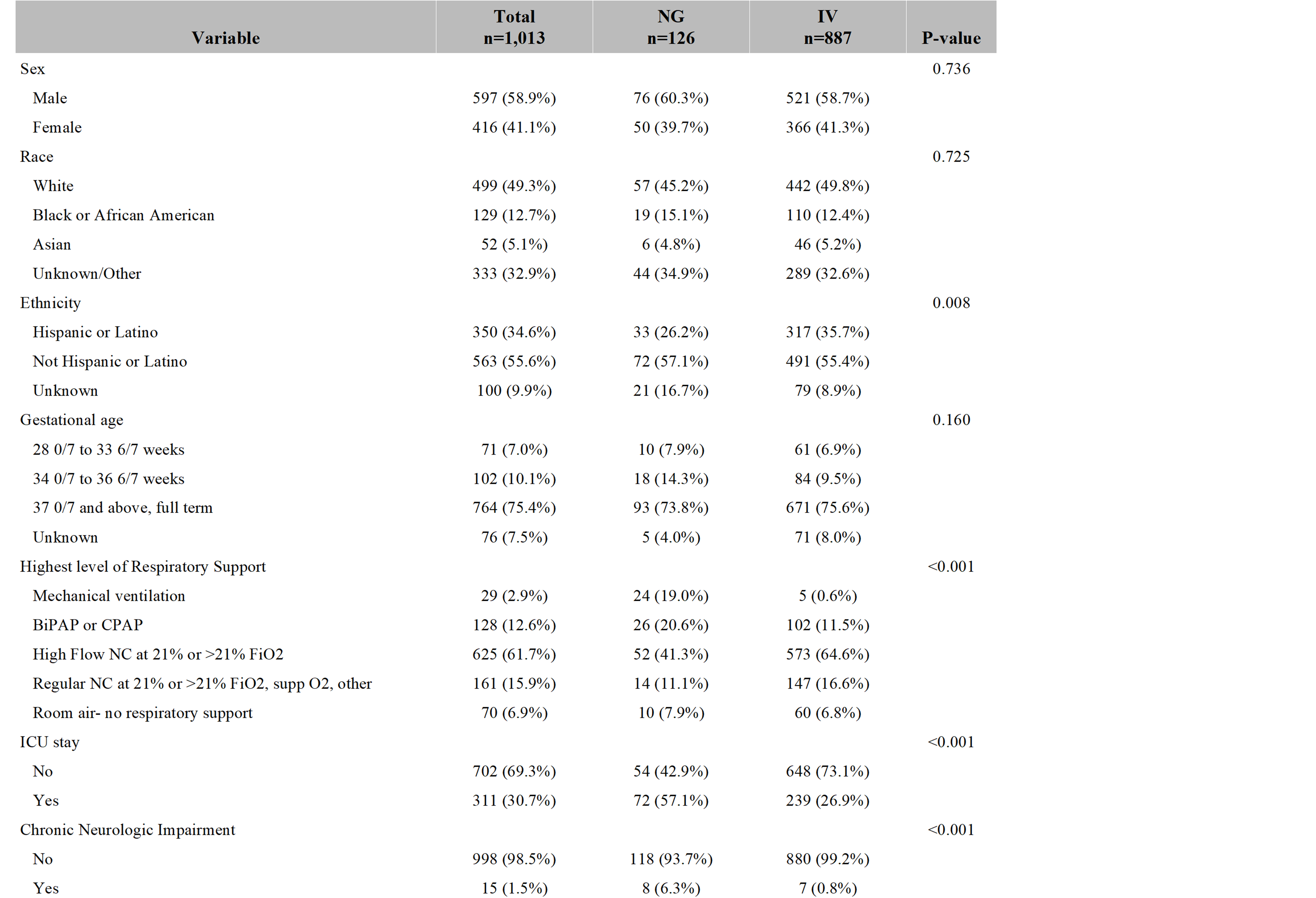
Design/Methods: This observational multicenter sub-study added questions to the Eliminating Monitor Overuse (EMO) study’s data collection form asking if the patient received NG, intravenous (IV), or Subcutaneous (SubQ) fluids for hydration or nutrition during their hospitalization. Patients were observed between January and May 2023 and population included a convenience sample of children 2 through 23 months on a general hospital medicine service with active primary diagnosis of bronchiolitis. Those with extreme prematurity (defined as < 28 weeks), documented apnea or cyanosis during the current illness, or complex chronic condition (defined as cardiac disease, pulmonary hypertension, chronic lung disease, home oxygen requirement, neuromuscular disease, immunodeficiency, cancer, or known or suspected Covid-19) were excluded. Any fluids or feeds administered via the NG or IV route were considered hydration, excluding those used for medication administration or electrolyte repletion fluids (e.g., KPhos or flushes). The primary outcome was NG hydration utilization. Clinical factors were compared between the NG and IV cohorts using Pearson Chi-Square and Fishers Exact tests.
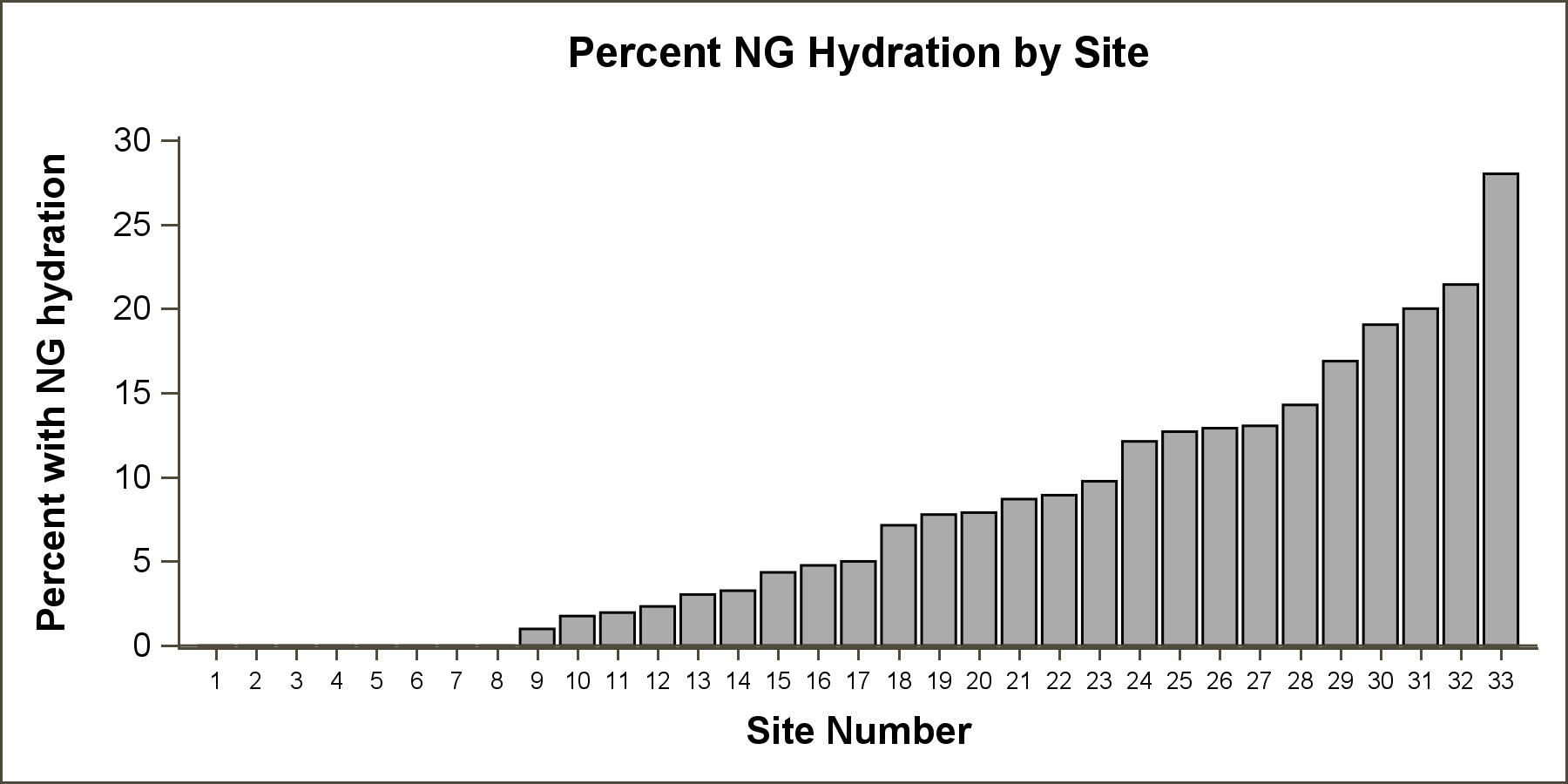
Results: There were 2,101 unique observations in the main study from 36 hospitals. Our sub-study included 1,720 observations from 33 hospitals that answered our study question and after exclusions for missing data. Of those, overall NG utilization was 7.3%, with institution utilization rates ranging from 0% to 28%. In patients who received NG hydration, they were more likely to receive mechanical ventilation, stay in the ICU, and have neurologic impairment.
Conclusion(s): We found a wide variation of NG hydration use amongst bronchiolitis patients, with lower use of NG hydration compared to IV hydration. NG hydration was more prevalent with mechanical ventilation, ICU stay, and neurologic impairment, suggesting a preference for initiating NG in critically ill, medically complex children. Future analysis is necessary to understand underuse and variability of NG hydration in otherwise healthy children.