Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 3
8 - Improving inpatient discharge efficiency through enhanced communication strategies (alone)
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 8
Publication Number: 8.3212
Publication Number: 8.3212

Daniela Hochreiter, MD (she/her/hers)
Associate Professor of Clinical Pediatrics
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Efficient patient flow and throughput are crucial to patient safety. Patients discharged during times of high inpatient volumes/patient surges face higher rates of readmissions, emergency department (ED) revisits, and mortality. In response to fluctuating patient volumes caused by the COVID-19 pandemic and following surges due to respiratory viruses, our tertiary care inpatient units observed a decline in patients being discharged before 11 AM.
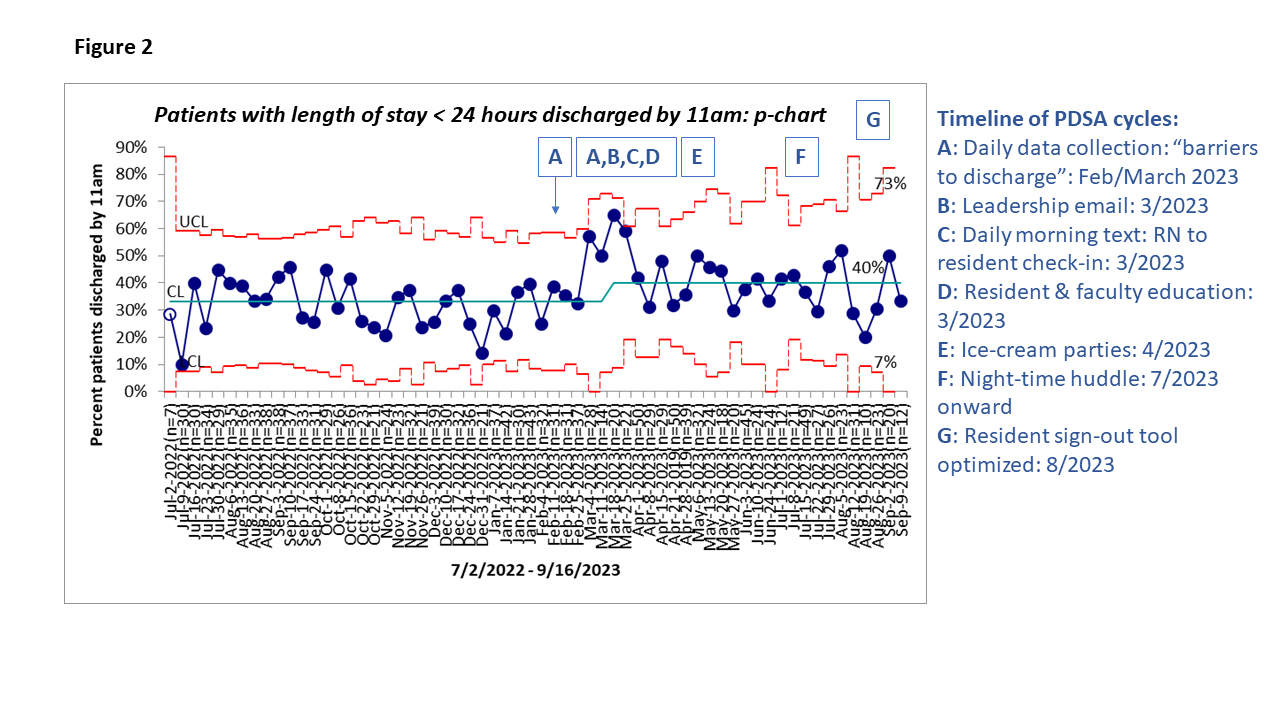
Objective: Through quality improvement methodology, we aimed to increase discharges before 11 AM for medical patients with length of stay (LOS) >24 hours and < 24 hours from 24% to 30%, and 33% to 40%, respectively, over a 1-year period.
Design/Methods: A multidisciplinary team of nurses, care managers, patient representative, electronic medical record (EMR) specialist, chief residents, and hospitalists was formed. Pareto analysis helped identify barriers to timely discharge. Iterative plan-do-study-act cycles centered on enhanced nurse-physician communication through the initiation of a night-time huddle, consistent morning texts, scripts and re-structuring of afternoon care management and resident huddle, staff engagement through feedback on barriers to discharge, motivational leadership email, and optimization of a sign-out tool used by residents. Outcome and process measures were analyzed on process control charts.
Results: We included 647 patients over a 14-month period. Surgical and behavioral health patients were excluded. Pareto analysis showed that prescription delays, communication breakdown, and lack of transportation were the most common barriers to timely discharge (Figure 1). Special cause was achieved within 3 months for patients with LOS < 24 hours with a center line shift from 33% to 40% percent, which has been sustained (Figure 2); no improvement has yet been shown for patients with LOS > 24 hours. Balancing measures, LOS, and 30-day readmissions, remained stable.
Conclusion(s): Discharge efficiency for patients with shorter LOS was improved through enhanced communication strategies alone. It is likely that patients with LOS > 24 hours have higher medical complexity and added barriers to discharge. Future process improvement work will therefore focus on testing higher-reliability interventions such as the integration of a discharge pathway and checklist into the EMR along with active involvement of caregivers in the discharge process.
.png)