Hospital Medicine
Session: Hospital Medicine 2
323 - Inter-hospital Transfers from Inpatient Pediatric Rehabilitation to Acute Care: Sociodemographic and Clinical Factors
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 323
Publication Number: 323.183
Publication Number: 323.183

Suzanne Rybczynski, MD, MSHCM (she/her/hers)
Chief Medical Officer
East Tennessee Children's Hospital
Knoxville, Tennessee, United States
Presenting Author(s)
Background: Youth receiving care in an acute inpatient pediatric rehabilitation hospital are among the most medically complex pediatric patients. Transfers pose a potential patient safety concern given risk of moving an unstable or critically ill child along with the risk of inter-hospital handoff communications. To mitigate the risk inherent to these transfers, analysis of patient sociodemographic and clinical factors could help to anticipate patients most at risk for transfers. This could influence changes to clinical practice with the goal of preventing transfers.
Objective: The purpose of this study was to evaluate which patients were more likely to require unplanned transfer to acute care considering clinical and sociodemographic factors.
Design/Methods: Our study is a single-site retrospective chart review using a convenience sample of all patients admitted to our inpatient pediatric rehabilitation hospital from January 2017 to May 2022. We used descriptive statistics and chi-square tests to compare patients’ sociodemographic and clinical factors between all admissions and transfer cases.
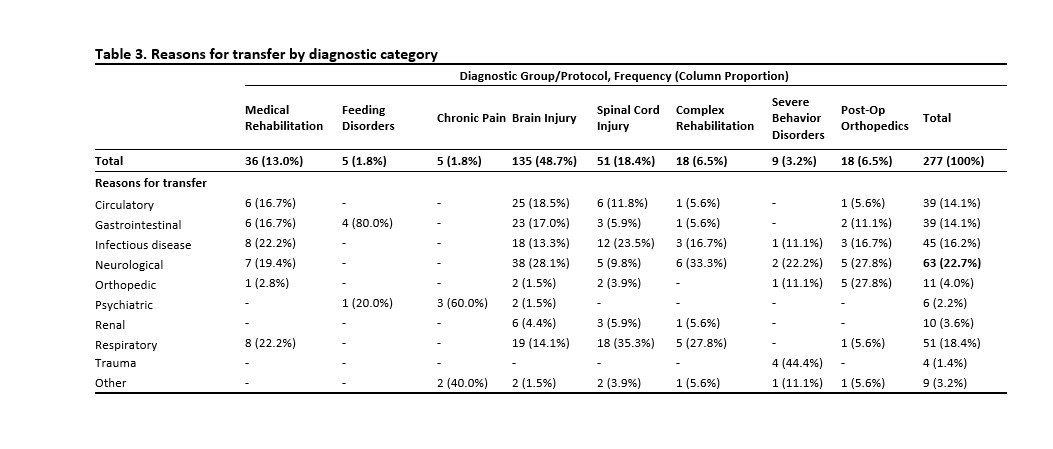
Results: There were 1375 unique patients included in the study. A significantly higher proportion of patients admitted were male (56.2%), non-Hispanic/Latino (85.0%), had private insurance (52.5%), and spoke English (92.1%). We found no statistically significant differences in sex, insurance coverage, and preferred language when comparing all admissions to transfer events. Hispanic patients and those who required interpreter were associated with a lower proportion of transfers. (Table 1) Patients with brain injury were both the most frequently admitted (22.6%) and transferred diagnostic group (48.7%). (Tables 2 & 3)
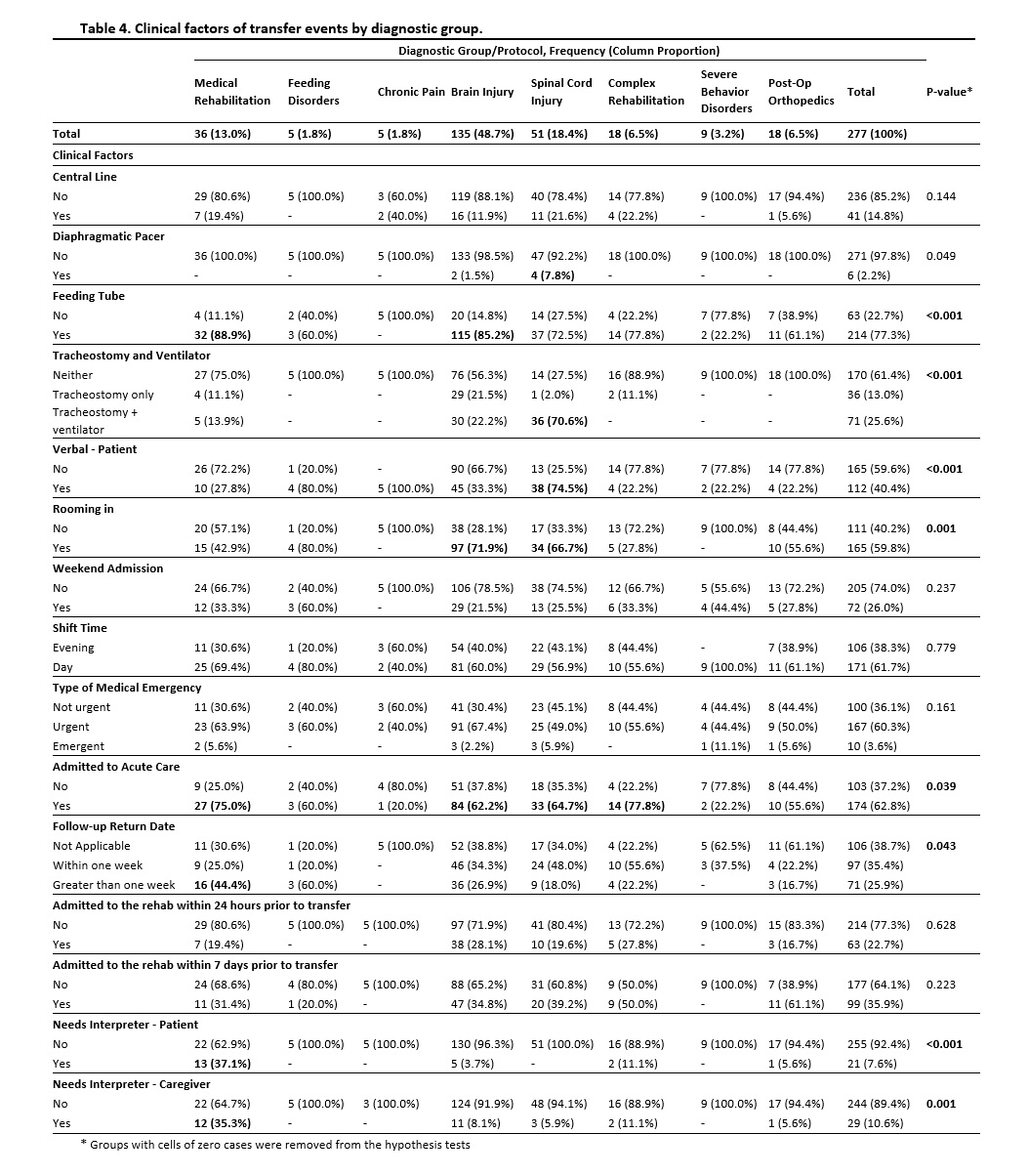
There were 174 unique patients involved in 277 transfers; 34% (N=60) had multiple transfers. The most common reason for transfer was due to a neurological (22.7%) concerns. (Table 3) Most events were on day shift (61.7%) and weekdays (74.0%) with 62.8% resulting in admission to acute care. Most patients had a feeding tube (77.3%), were non-verbal (59.6%), and had a caregiver present (59.8%). Except for the medical rehabilitation group, most transferred patients and their caregivers did not need an interpreter. (Table 4)
Conclusion(s): We identified demographic and clinical factors associated with admissions and transfers to higher level of care of pediatric rehabilitation, which might help further understanding of potential risk factors leading to inter-hospital transfers. Focusing on groups at higher risk may allow medical personnel and caregivers to take preventative measures to transfers.
.jpg)