Hospital Medicine
Session: Hospital Medicine 4
139 - Improving Physician and Bedside Nurse Communication through Patient Arrival Huddles
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 139
Publication Number: 139.1525
Publication Number: 139.1525

Britanny Winckler, MD, MBA
Assistant Clinical Professor
University of California, Irvine, School of Medicine
Orange, California, United States
Presenting Author(s)
Background: Communication failures, particularly when patients transition between care settings, are leading causes of medical errors and sentinel events.1-2 The perception of inadequate intradisciplinary communication have been demonstrated to be a key driver in low patient satisfaction scores. Efforts to standardize handoffs have led to improvements in patient safety and experience.3
Objective: To improve the rate of structured communication huddles between the bedside nurse and admitting medical team on the acute care unit within two hours of a new admission from 0% to 70% within one year.
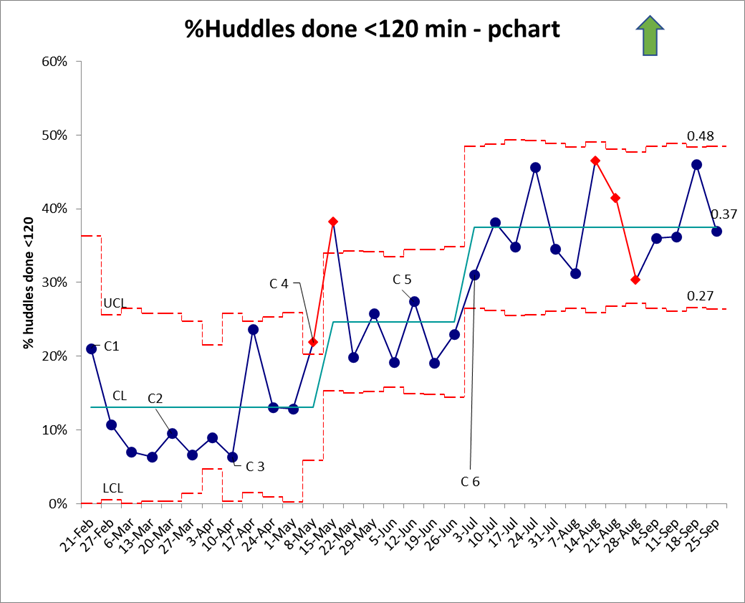
Design/Methods: An interprofessional team of physicians (including trainees) and nurses at our free-standing suburban children’s hospital collaborated to apply improvement science methodology including a process map and cause and effect and key driver diagrams. The primary measure was the percentage of patients with a completed arrival huddle within two hours of patient arrival (process). Additional measures included the number and staff perception of handoff communication errors (outcome) and nurse and resident satisfaction and perceived impact on other duties (balancing). Plan-Do-Study-Act (PDSA) cycles were initiated in February 2023. C1: Initiation of the huddle for patients on one resident team. C2: Arrival pages sent directly from the unit to the admitting team. C3: Huddles expanded to additional daytime resident team. C4: Huddles expanded to all teams at all times of the day. C5: Admit nurses completed an assessment of barriers. C6: Huddles included as a workflow expectation during new intern orientation. Nurse surveys were conducted during C1-4.
Results: The rate of patients with arrival huddles was 13.1% during C1-3. After C4, special cause variation was noted with a centerline shift to 24.7% (Figure 1). Special cause variation occurred again after C6 with a centerline shift to 37.5%. Surveys revealed that nurses believe patient huddles are important to patient care, transfer of knowledge, and building relationships. They also acknowledged the presence of competing priorities and difficulty coordinating patient arrivals, which poses a challenge to timely huddles.
Conclusion(s): While we have made progress in increasing the completion rate of timely bedside huddles, room for improvement remains as we have not yet achieved our aim. Next steps include 1) planned experimentation using full factorial design to pinpoint areas for further improvement and 2) analyzing data for outcome and balancing measures.