Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 4
257 - Identifying Demographic Disparities in Emergency Department Utilization Among Primary Care Patients
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 257
Publication Number: 257.1521
Publication Number: 257.1521

Jessica C. Martin, MD (she/her/hers)
Clinical Fellow
Boston Children's Hospital
Cambridge, Massachusetts, United States
Presenting Author(s)
Background: Because emergency department (ED) visits can indicate poor health and reduced access to alternative forms of care, rates of ED utilization are used as a primary care quality indicator. To launch an equity-focused quality improvement initiative we sought to understand the disparities in visit rates among the patient population in two aligned primary care clinics.
Objective: To describe disparities in ED visit rates among primary care patients
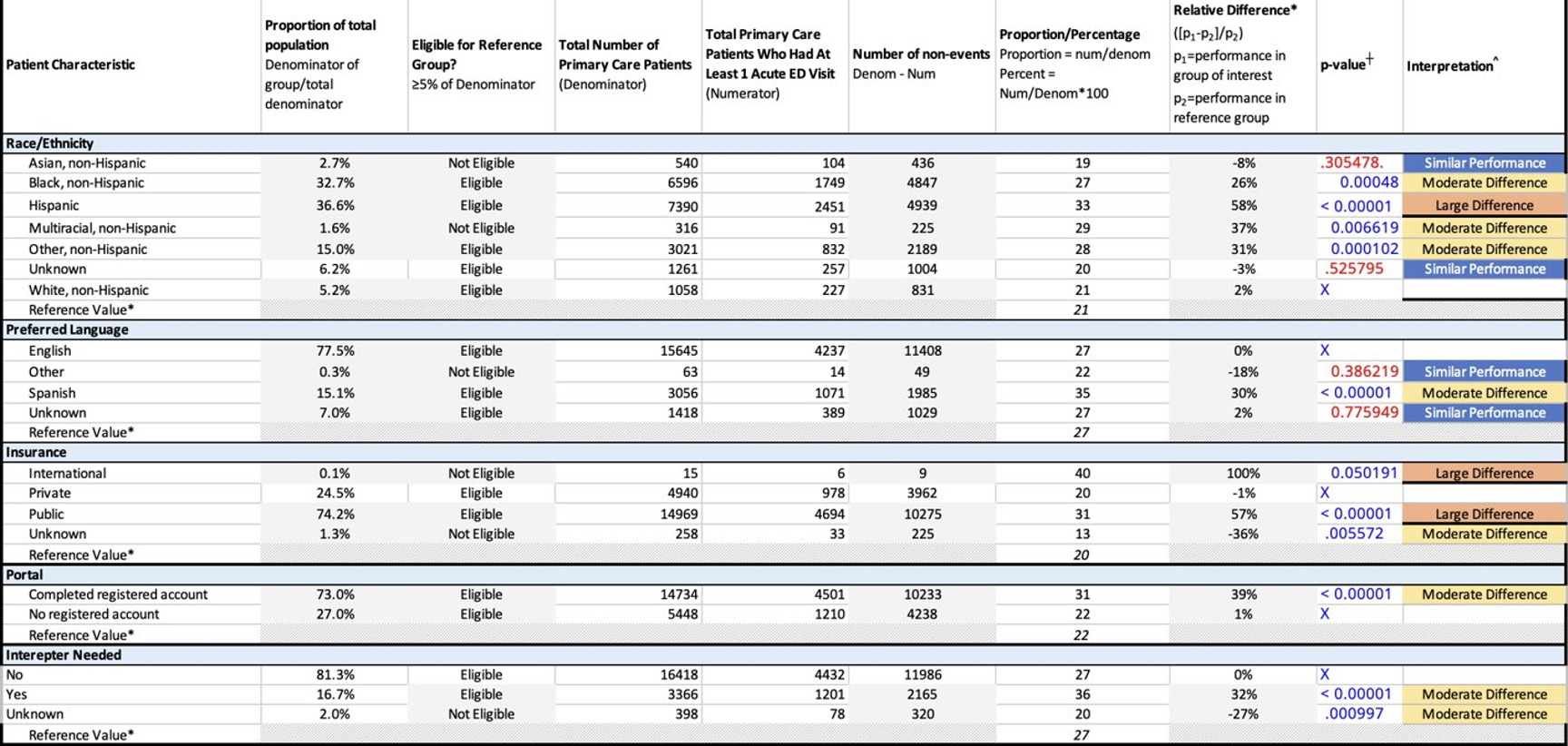
Design/Methods: We retrospectively examined ED utilization for all Boston Children’s Hospital (BCH) primary care patients between November 2021 and January 2023. We examined the proportion of patients with at least one billed visit to the BCH ED, stratified by demographic characteristics including race/ethnicity, language, insurance status, and utilization of the patient portal, as a proxy for accessing medical advice. We utilized a combination of relative difference and chi-square to determine differences between groups; we interpreted p values ≤0.10 and relative differences of ±10%, ±11-40%, and ±>40% as similar, moderate, and large difference respectively. Reference group was chosen as that representing more than 5% percent of the population with the lowest proportion who visited the ED.
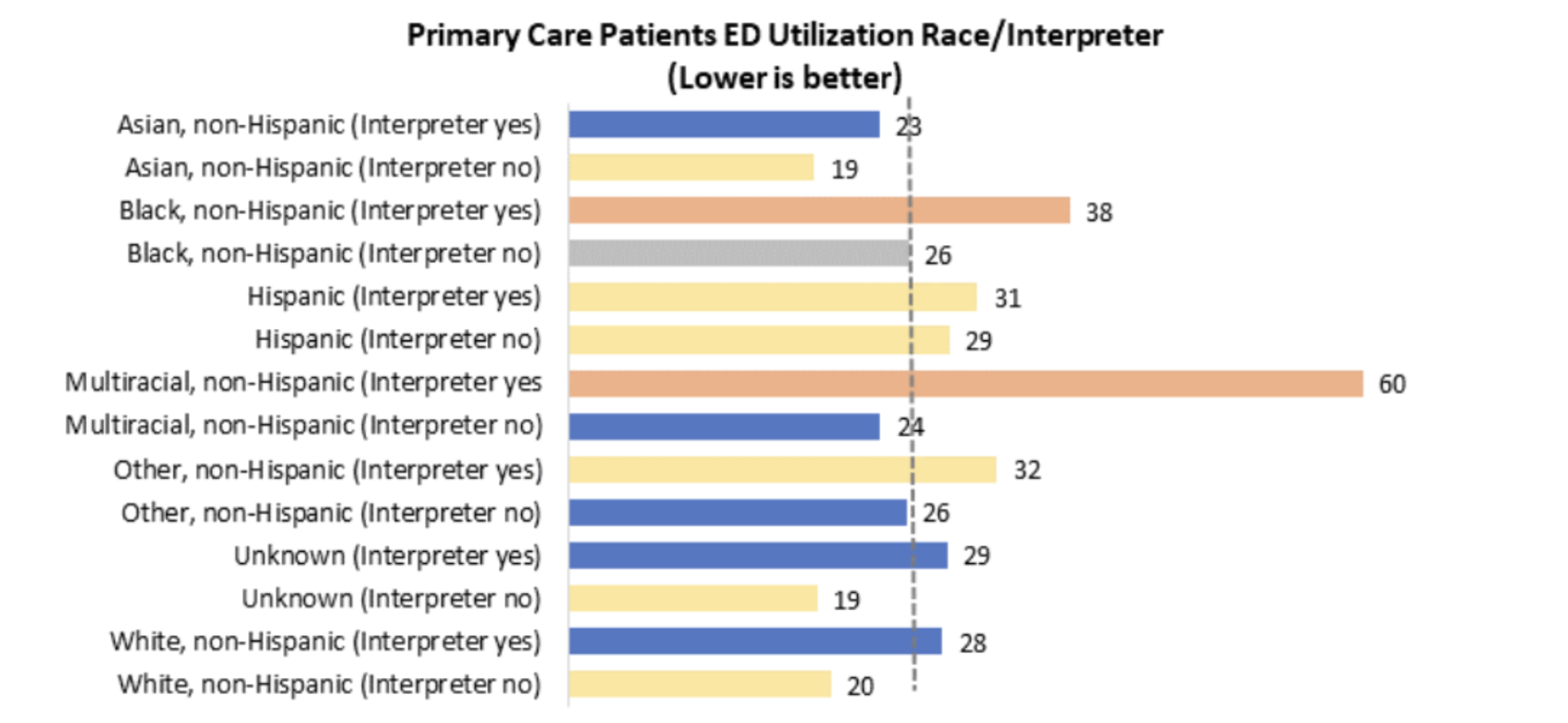
Results: Overall, 28% of our population (n=20182) had at least one ED visit in the interval. We found statistically significant differences in ED utilization between subgroups categorized by race/ethnicity, preferred language, need for an interpreter, and insurance type, though not by portal usage. A higher proportion of Hispanic patients visited the ED compared to White/non-Hispanic patients (33 versus 21%, p< 0.01), and there were moderate differences between Black/non-Hispanic, Multiracial/non-Hispanic, and White/non-Hispanic patients (27 versus 21%, p < 0.01 and 29 versus 21%, p< 0.01, respectively). In a stratified analysis combining race/ethnicity and need for an interpreter, one of the largest statistically significant differences in ED utilization occurred in the Black, non-Hispanic, interpreter needed population compared to other race, non-Hispanic, no interpreter needed (38 vs. 20%, p < 0.05).
Conclusion(s): Among BCH primary care patients, those who identify as Hispanic, Black, or Multiracial, and those needing an interpreter are more likely to use the ED, suggesting that interventions to reduce disparities in ED utilization should focus on improving services for these populations. Next steps include qualitative work to understand and address drivers of ED utilization and attempts to understand the effect of past interventions on different subgroups.