Technology
Session: Technology 1
171 - NeoConnect: TeleRounds for Tiny Ones
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 171
Publication Number: 171.1836
Publication Number: 171.1836

Thea DeBroux (she/her/hers)
Undergraduate Research Assistant
University of Washington Department of Pediatrics
San Diego, California, United States
Presenting Author(s)
Background: Extremely preterm (EP) infants, born 22 0/7-24 6/7 weeks' gestational age are a subset of babies cared for at the University of Washington (UW) NICU. A night telerounds program was initiated in July 2022, to support the bedside team caring for critically ill and EP neonates. There are no descriptions of night telerounds in level IV academic NICUs.
Objective: To evaluate the feasibility of night telerounds in a level IV NICU for EP neonates before and after implementation.
Design/Methods: This study was a retrospective review of electronic medical records, EP database and telemedicine records. Night telerounds involved the on-call attending joining bedside night rounds on critically ill patients using a Teladoc™ cart. Frequency and duration of telerounds within the second shift (8-11pm) was analyzed. Data on EP outcomes was compared between two epochs: pre- (Jul 2021-Jun 2022); and post-night telerounds implementation (Jul 2022-Jun 2023). Descriptive statistics, chi square and independent samples t-test were used to compare EP outcomes between epochs.
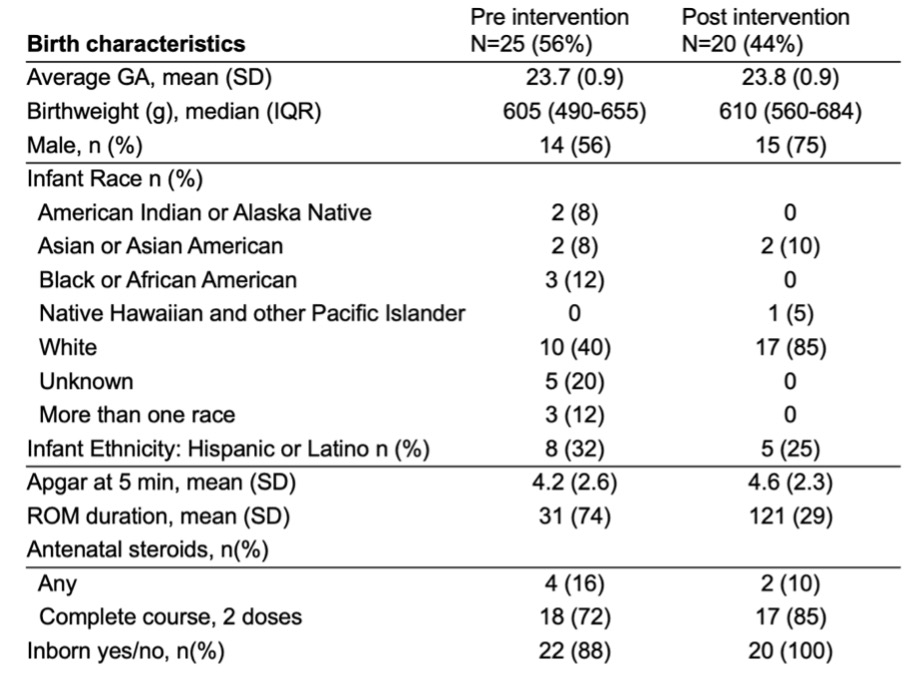
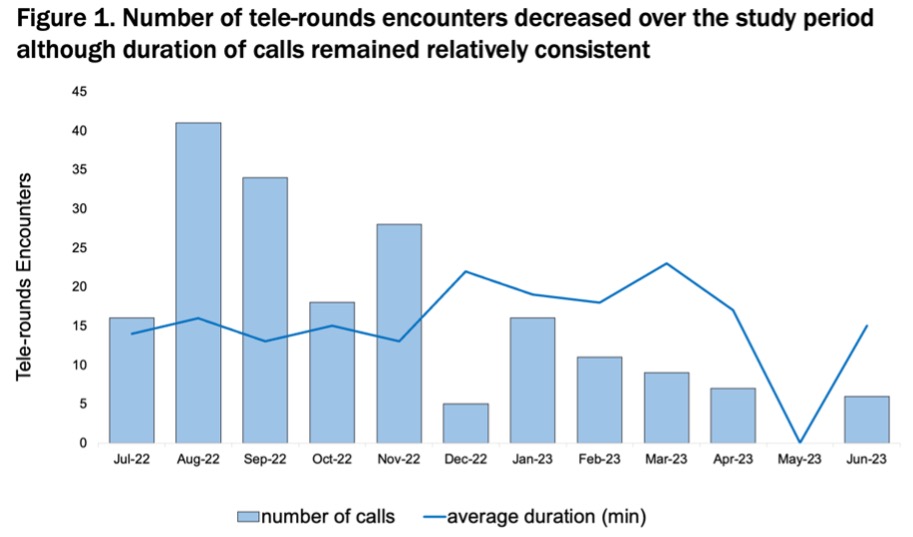
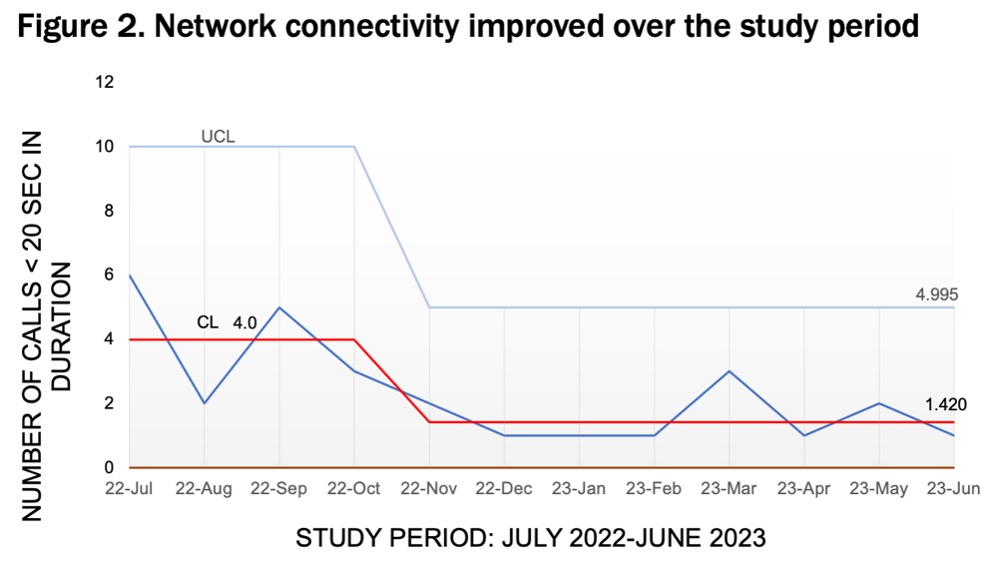
Results: From Jul 2021-Jun 2023, 45 EPs were admitted to UW NICU (25 pre and 20 post-night telerounds implementation). See Table 1. There were 195 night telerounds encounters during the study period with a median of 14 (IQR 7-21) encounters/month. The median duration of encounters was 16 (IQR 14-18) minutes (Figure 1). Network connectivity issues, defined as calls lasting < 20 sec in duration, improved during the study period (Figure 2). Prior to night tele-rounds, 9 (36%) of EPs were transferred for subspecialty/surgical care, mortality before 36 weeks’ post-menstrual age (PMA) was 14 (56%) and median length of stay (LOS) for survivors to discharge was 182 days (SD 72). After implementing telerounds, 10 (50%) EPs were transferred with mortality before 36 weeks’ PMA of 7 (35%) and median LOS for survivors to discharge was 139 days (SD 24). There was a trend towards reduced total days of ventilation (invasive + non-invasive) (176, SD 77 vs 121, SD 29; p=0.05). Additional chart review on orders entered during night rounds is being conducted.
Conclusion(s): Night telerounds are feasible to support the bedside NICU team caring for critically ill neonates. Attending neonatologist participation in night rounds may facilitate advancing care. More studies are needed to evaluate the impact and acceptability of this intervention.