Neonatology
Session: Neo-Perinatal Health Care Delivery 3: Epidemiology/Health Services Research
261 - Impact of teleneonatology on time to goal temperature in outborn neonates treated with therapeutic hypothermia for hypoxic-ischemic encephalopathy
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 261
Publication Number: 261.1840
Publication Number: 261.1840

Mark W. Kaczor, MD (he/him/his)
Neonatal-Perinatal Medicine Fellow
Mayo Clinic Children's Center
Rochester, Minnesota, United States
Presenting Author(s)
Background: Neonates with hypoxic-ischemic encephalopathy (HIE) that require transfer to a neonatal intensive care unit (NICU) for therapeutic hypothermia (TH) have higher rates of morbidity and mortality compared to neonates born in a hospital with an NICU. It is unknown whether support of referring hospital care teams via real-time, audio-video telemedicine consults with a neonatologist (termed “teleneonatology”) impacts the timeliness of TH initiation or early neurologic outcomes compared to neonates managed with usual care.
Objective: To assess whether teleneonatology reduces time to goal temperature in neonates with HIE requiring transport to an NICU for TH.
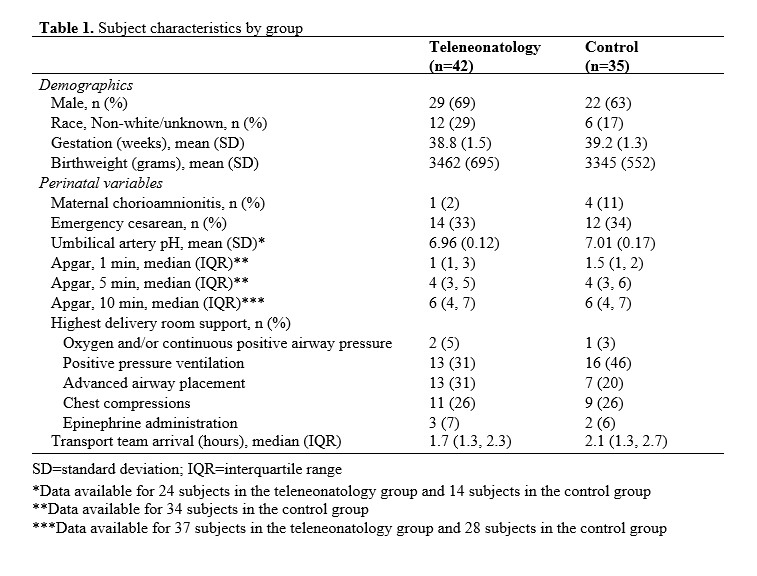
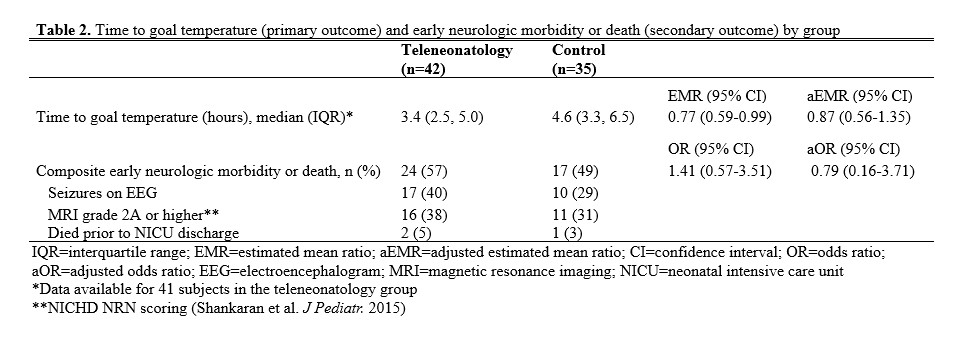
Design/Methods: This retrospective cohort study at a single center included neonates born from February 2013 to November 2022. Those born outside a hospital birthing unit or for whom neonatal transport was present at delivery were excluded. The intervention group included neonates that received teleneonatology consultation during initial resuscitation; the control group did not. The primary outcome was time from birth to achievement of goal temperature (33-34 degrees C). The secondary outcome was a composite of early neurologic morbidity or death, which included electrographic seizures, evidence of significant brain injury on MRI (grade 2A or greater), and in-hospital mortality.
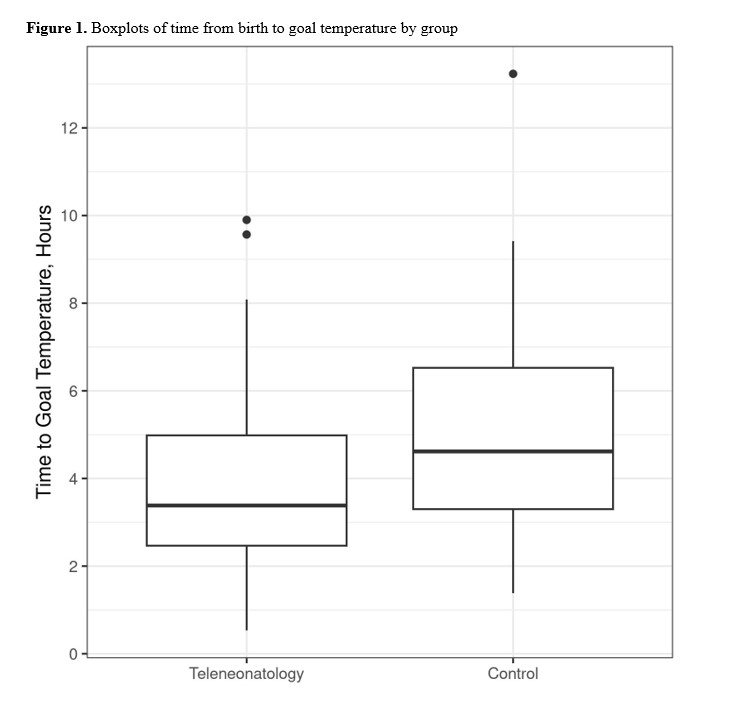
Results: The neonates in teleneonatology group (n=42) and control group (n=35) were generally similar (Table 1). Median (IQR) time from birth to goal temperature was lower in the teleneonatology group compared to the control group (3.4 [2.5, 5.0] vs 4.6 [3.3, 6.5] hours; estimated mean ratio 0.77; 95% CI, 0.59-0.99, Figure 1). This effect was no longer significant when adjusting for time from birth to transport team arrival, maternal chorioamnionitis, and umbilical cord arterial pH. Interaction testing did not demonstrate a difference in the association of time to transport team arrival and time to achievement of goal temperature between the groups. Teleneonatology was not associated with a difference the composite outcome of early neurologic morbidity or death in unadjusted or adjusted analyses (Table 2).
Conclusion(s): Teleneonatology consultation may reduce the time from birth to achievement of goal temperature in neonates requiring transport to an NICU for TH. Further multi-site, prospective research with larger sample sizes and adequate controlling for confounding is needed to clarify this issue.