Neonatology
Session: Neonatal Quality Improvement 5
78 - Implementation of 2022 AAP Guidelines Optimizes Neonatal Hyperbilirubinemia Healthcare Utilization
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 78
Publication Number: 78.3179
Publication Number: 78.3179

Michaela A. Simpson, MD (she/her/hers)
Pediatric Resident Physician
Medical College of Wisconsin
Wauwatosa, Wisconsin, United States
Presenting Author(s)
Background: The 2022 AAP Neonatal Hyperbilirubinemia (NH) guidelines for risk assessment, monitoring, and treatment of newborns ≥ 35 weeks gestation include revised monitoring and treatment recommendations to focus healthcare utilization on infants with high-risk NH at risk of kernicterus. Implementation required coordination and culture change across healthcare settings, specifically for infants requiring phototherapy (PT).
Objective: Our SMART AIM was to optimize healthcare utilization and care for infants receiving PT during birth hospitalization at our academic newborn nursery (NBN) by intervening on the right infant at the right time according to the 2022 AAP NH guidelines without increasing PT and lab utilization burden on infants, the institution, or surrounding health systems.
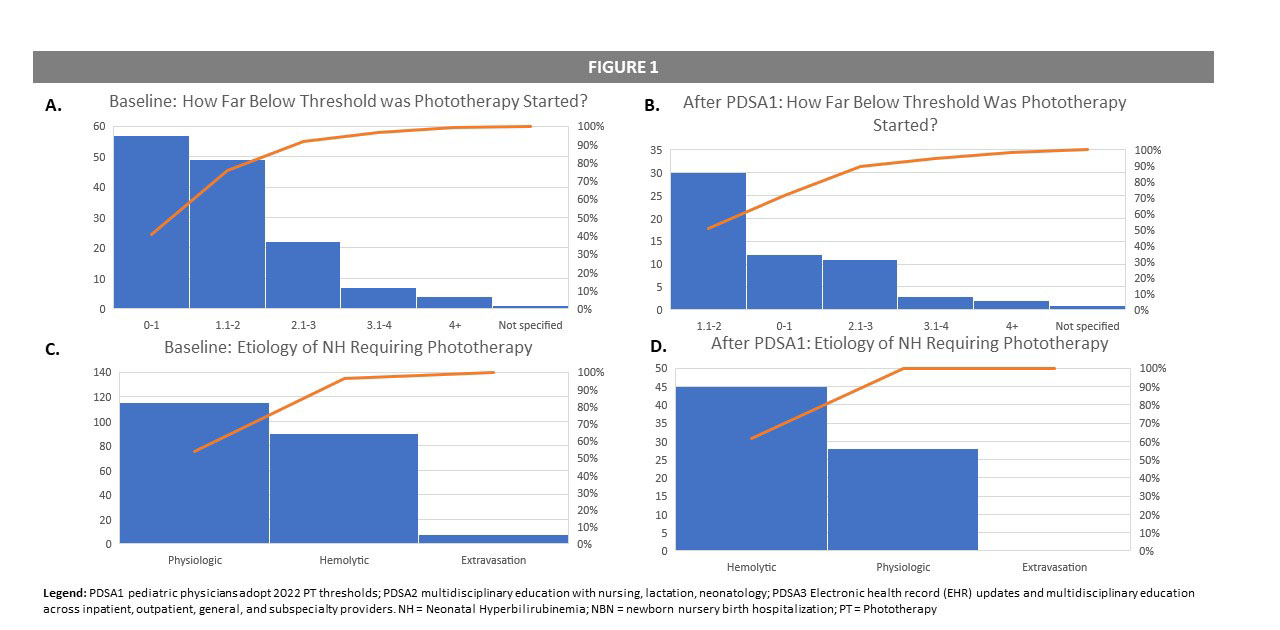
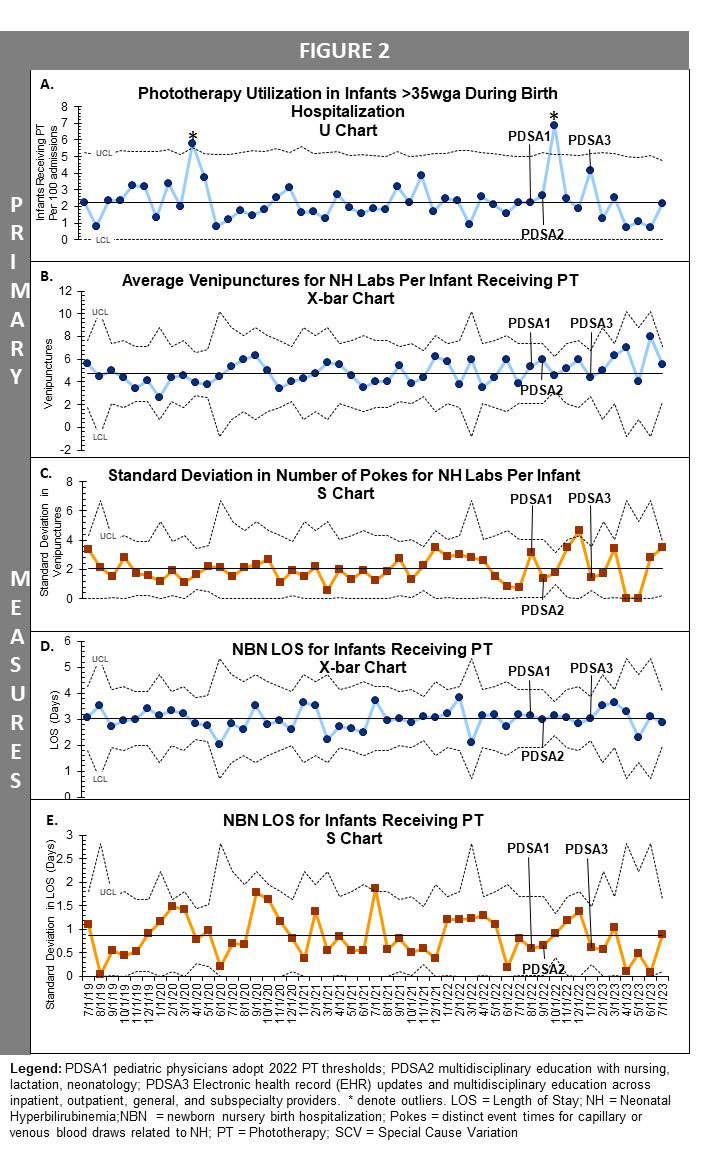
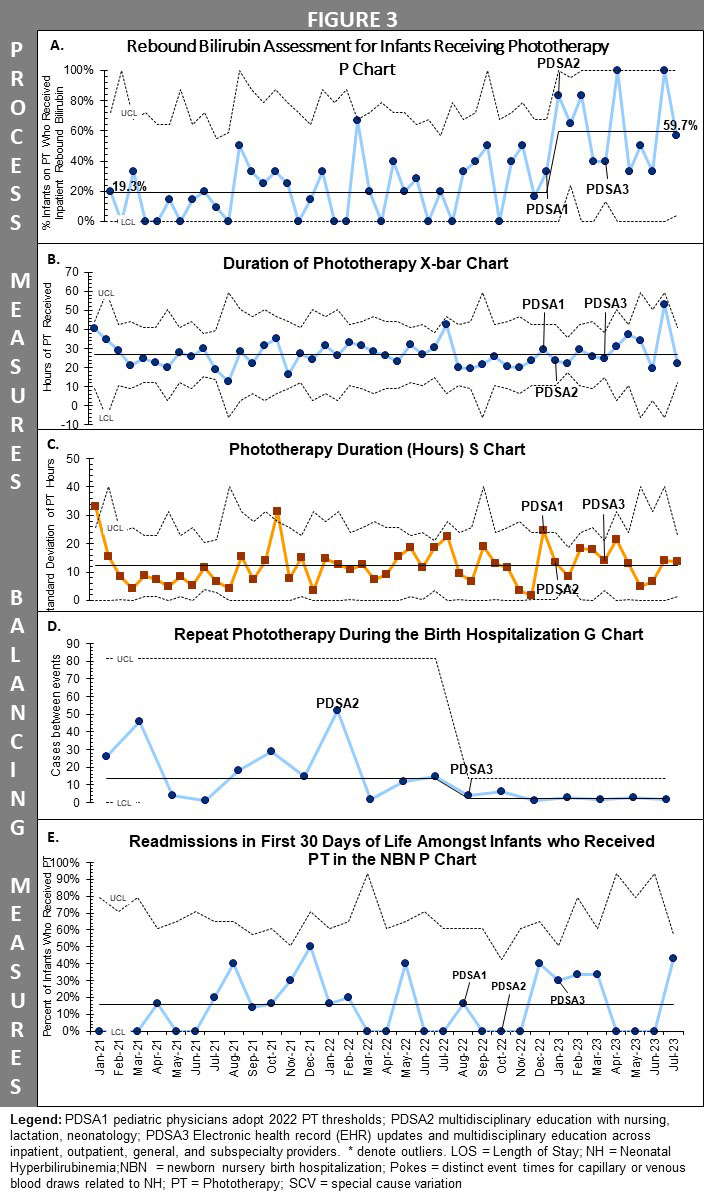
Design/Methods: Infants ≥ 35 weeks gestation admitted to and discharged from our NBN who received PT from July 2019 to July 2023 were included. Exclusion criteria included transfer to NICU, PT outside of the NBN, and death. Key driver diagram and Pareto chart analysis of baseline data guided selection of PDSA cycles which started in August 2022. Primary, process and balancing measures were tracked monthly. Primary outcome measures were PT utilization, NH-related venipunctures, and length of stay (LOS). Process measures included rebound TSB assessment and duration of PT. Balancing measures were instances of repeat PT during the NBN stay and readmissions within 30 days of birth for NH at our hospital system or nearby pediatric referral center. Process control charts were made with Excel QI Macros and special cause variation (SCV) was defined by Shewhart rules.
Results: Baseline data analysis demonstrated the majority of infants receiving PT had PT initiated when total bilirubin was within 2mg/dl of PT threshold, and for treatment of physiologic NH. After PDSA#1, most infants in our NBN receiving PT had hemolytic rather than physiologic NH (Figure 1). Despite this shift in treatment cohort, primary outcome measures did not demonstrate SCV (Figure 2). Process measures showed increased variability, including SCV in rebound bilirubin assessment. Frequency of repeat PT during NBN stay increased, but readmissions did not (Figure 3). Transfers to NICU for NH did not increase.
Conclusion(s): We achieved our aim of updating NH management through robust education and EHR updates to standardize care. Infants with hemolytic risk factors are now the principal cohort of those receiving PT. Despite increasing rebound bilirubin assessments and repeat PT during NBN stay, primary measures of healthcare utilization have not increased.