Emergency Medicine
Session: Emergency Medicine 10: Trauma
392 - Assessing Care Delivery for Children with Mild Traumatic Brain Injury in the ED using Group Model Building
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 392
Publication Number: 392.3175
Publication Number: 392.3175

Pradip P. Chaudhari, MD (he/him/his)
Attending Physician
Children's Hospital Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Despite evidence supporting guideline-based care in improving mild traumatic brain injury (mTBI) outcomes, adherence remains inconsistent. Proper adherence is contingent upon interplay of guideline specifications, institutional nuances, and actions of providers. Group model building (or community-based system dynamics, GMB) is a rigorous implementation science methodology for engaging stakeholders by leveraging their knowledge of a given system from an endogenous feedback perspective. This allows for the establishment of a shared mental model, stakeholder buy-in, and identifying leverage points for feasible and successful intervention.
Objective: Clinicians participated in a GMB session focused on care delivery for children with mTBI in the ED in which we aimed to (1) understand structural, site-specific factors contributing to workflow delays in information transfer and decision-making when caring for children with mTBI, including accessibility and use of established guidelines, and (2) identify key components of potential implementation strategies that may mitigate system-level sources of delays in information transfer and decision-making.
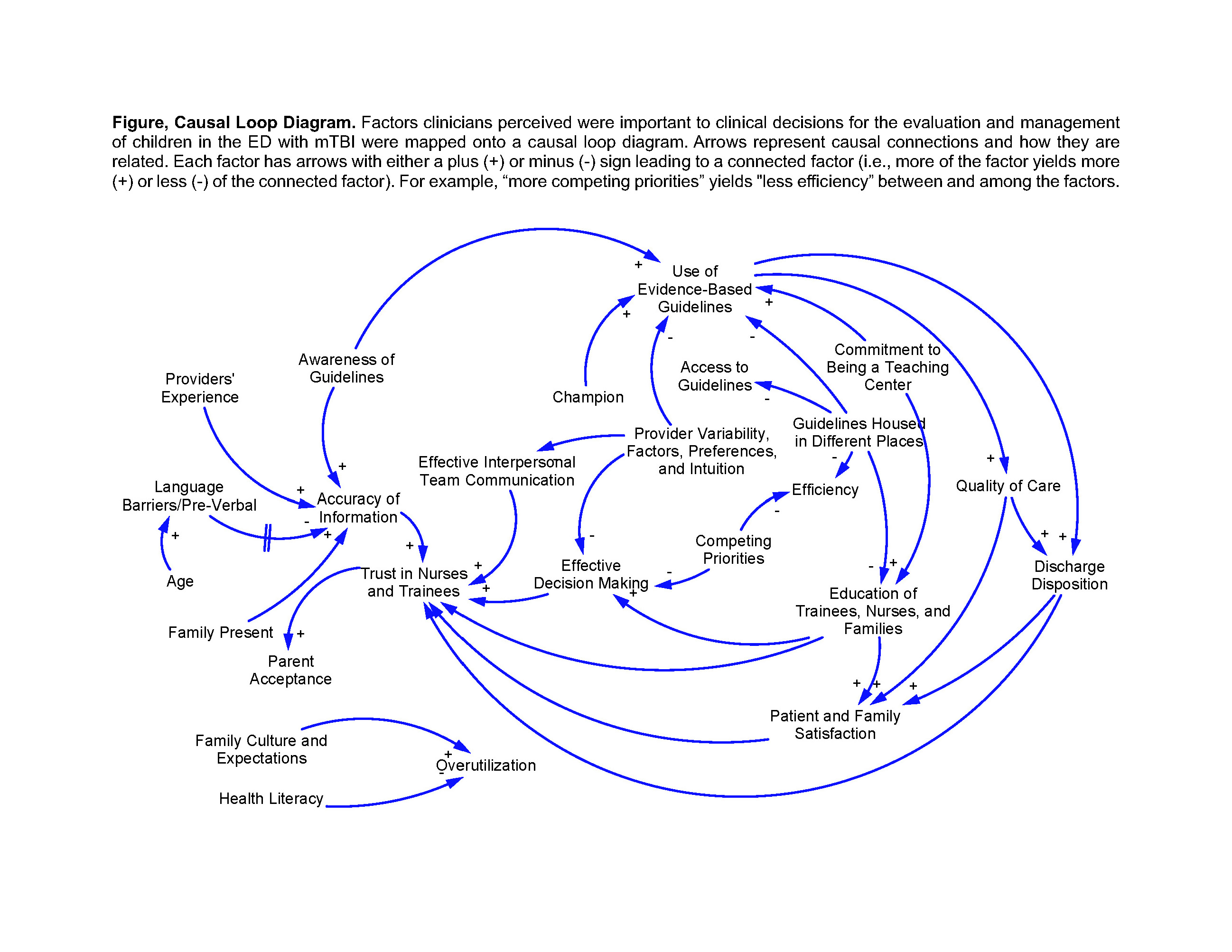
Design/Methods: We conducted a single center study utilizing a GMB approach. The process involved the design of a 2-hour, in-person workshop co-facilitated by an implementation scientist and clinician with expertise in mTBI management. The facilitation manual included standardized scripts for icebreaking, eliciting variables within the system, deliberating on how variables are connected, and voting on the most important variables. The GMB session yielded a causal loop diagram of the ED workflow for clinicians caring for children with mTBI. The diagram visually represents causal relationships and their relevance to pertinent factors.
Results: Among 8 workshop participants, 2 were pediatric emergency medicine (EM) clinical fellows and 6 were pediatric EM attendings. The causal loop diagram depicts several relevant system-level workflow factors that clinicians consider while managing children with mTBI including the role of trust during information gathering, ED patient volume, provider variability, and family expectations (Figure). For instance, clinicians noted that provider variability, including clinical preferences and intuition, may adversely impact effective decision making and the use of evidence-based guidelines.
Conclusion(s): The application of GMB was an innovative and effective approach for assessing ED context related to mTBI care. Results will be used to inform best practices for implementing evidence-based guidelines for children with mTBI within the ED.