Medical Education
Session: Medical Education 7
435 - Characterization of Resident Involvement in Neonatal Intubations
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 435
Publication Number: 435.1510
Publication Number: 435.1510

Samantha Shaffer, MD (she/her/hers)
resident
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Advances in neonatal care and changes in pediatric resident ACGME requirements have resulted in fewer opportunities for pediatric residents to participate in neonatal intubations.
Objective: We aimed to characterize baseline neonatal intubation practices and to examine IU resident involvement in neonatal intubations at one of our level III NICUs to act as a needs assessment for the design of a just-in-time neonatal intubation educational curriculum.
Design/Methods: We evaluated neonatal intubation procedure notes generated from the Electronic Medical Record (EMR) from January 2021 through July 2023 and excluded procedures that occurred in the delivery room. We recorded who was involved in each procedure, number of procedure attempts, use of video laryngoscopy, and potential reasons for resident non-involvement. If a pediatric or combined program resident was involved in the procedure, we documented their level of training and training program if available in the EMR.
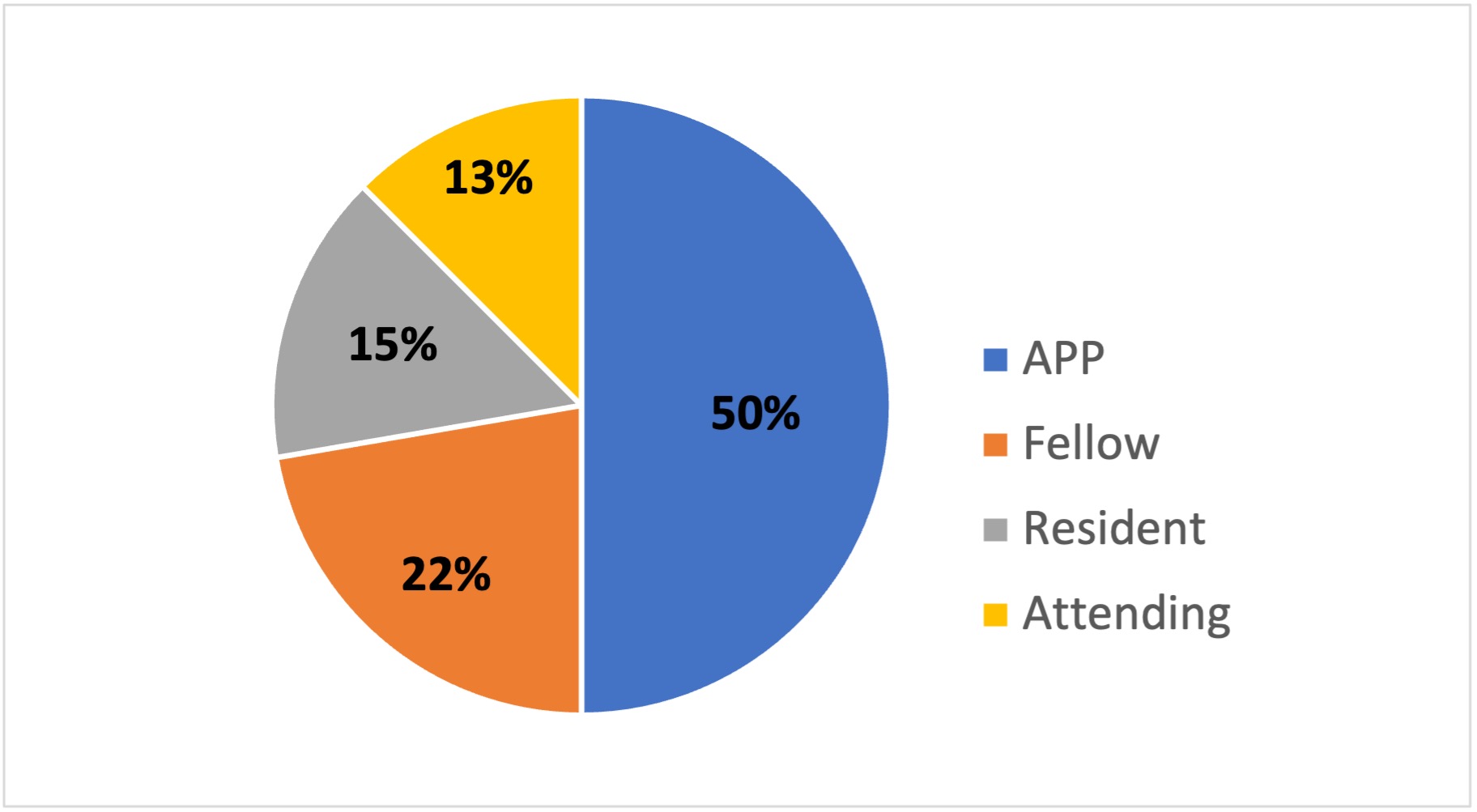
Results: There were 258 neonatal intubations from January 2021 through July 2023. Most procedures were successfully completed by advanced practice providers (APPs) (Figure 1). Pediatric or combined program residents were involved in 35% of procedures, with an overall resident success rate of 43%. First year residents were most involved in neonatal intubations (Figure 2) and together with third year residents shared the highest success rates (Figure 3). Although only a third of resident procedure attempts included video laryngoscopy, residents who used video laryngoscopy had an intubation success rate of 47% compared to 41% in those where video laryngoscopy was not used. Of the 167 neonatal intubations that did not involve residents, 49 (29%) were emergent, 93 (56%) were documented as patient weight < 1000g, incomplete pre-medication, or known congenital airway anomalies and 25 (15%) did not document a reason for resident non-involvement.
Conclusion(s): Residents had limited exposure to neonatal intubations and were successful in less than half of the procedures they were involved in. Similar procedure success rates between first and third year residents and improved success with use of video laryngoscopy suggests the ability to coach inexperienced learners through the procedure, creating opportunities for initiatives targeting improved resident procedure success despite limited exposure. We plan to use this data to develop a just-in-time intubation curriculum to improve procedure success rates for residents and other inexperienced providers.
.jpg)
.jpg)
