Neonatology
Session: Neonatal Nephrology/AKI 2
58 - The Relationship between Vitamin D (VitD) and Acute Kidney Injury (AKI) in Very Low Birth Weight (VLBW) Preterm Neonates
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 58
Publication Number: 58.1848
Publication Number: 58.1848

Molly J. Mead, BS (she/her/hers)
Medical Student
Medical University of South Carolina
Johns Island, South Carolina, United States
Presenting Author(s)
Background: Premature neonates are at increased risk for AKI which is independently associated with poor outcomes and increased mortality. Because of the conversion of 25(OH)D to the active hormone 1,25(OH)2D within the kidney, vitD deficiency likely is associated with kidney dysregulation. Limited studies have investigated associations between neonatal serum 25(OH)D, a marker for vitD status, and AKI. Fewer studies attempt to explore this relationship in VLBW ( < 1500g) neonates, a vulnerable population in the neonatal intensive care unit (NICU) at risk for vitD deficiency.
Objective: We aimed to investigate associations between neonatal serum 25(OH)D and AKI in a large cohort of VLBW neonates. We hypothesized that VLBW neonates with lower concentrations of serum 25(OH)D are more likely to develop AKI.
Design/Methods: We performed a chart review of VLBW neonates admitted to the NICU at MUSC between 2018-2020. Included in the present study are a subgroup of 60 neonates (from the original 567) who had measured serum 25(OH)D within 90 days of life (DOL).
In neonates with AKI, first reported AKI episode was used in this analysis, diagnosed using the modified, neonatal KDIGO creatinine criteria. If AKI occurred within the first 31DOL, median serum 25(OH)D, calculated from all available serum 25(OH)D measurements obtained during the first 31DOL, was investigated for associations with AKI. If AKI occurred after 31DOL, median serum 25(OH)D, calculated from all available serum 25(OH)D measurements obtained within ± 14 days of that AKI episode, was investigated for associations with AKI. In neonates without AKI, median serum 25(OH)D, calculated from all available serum 25(OH)D measurements obtained during the first 90DOL, was used.
Comparisons were made between those with and without AKI using chi-square (Fisher Exact Tests), Mann-Whitney U, and logistic regression. Association between serum 25(OH)D and AKI was evaluated using a logistic regression model.
Results: Of the 60 neonates, 21 (35%) developed AKI within 90DOL. Participant characteristics were similar between the groups apart from birth weight and 5-minute APGAR score (both p< 0.05, Table).
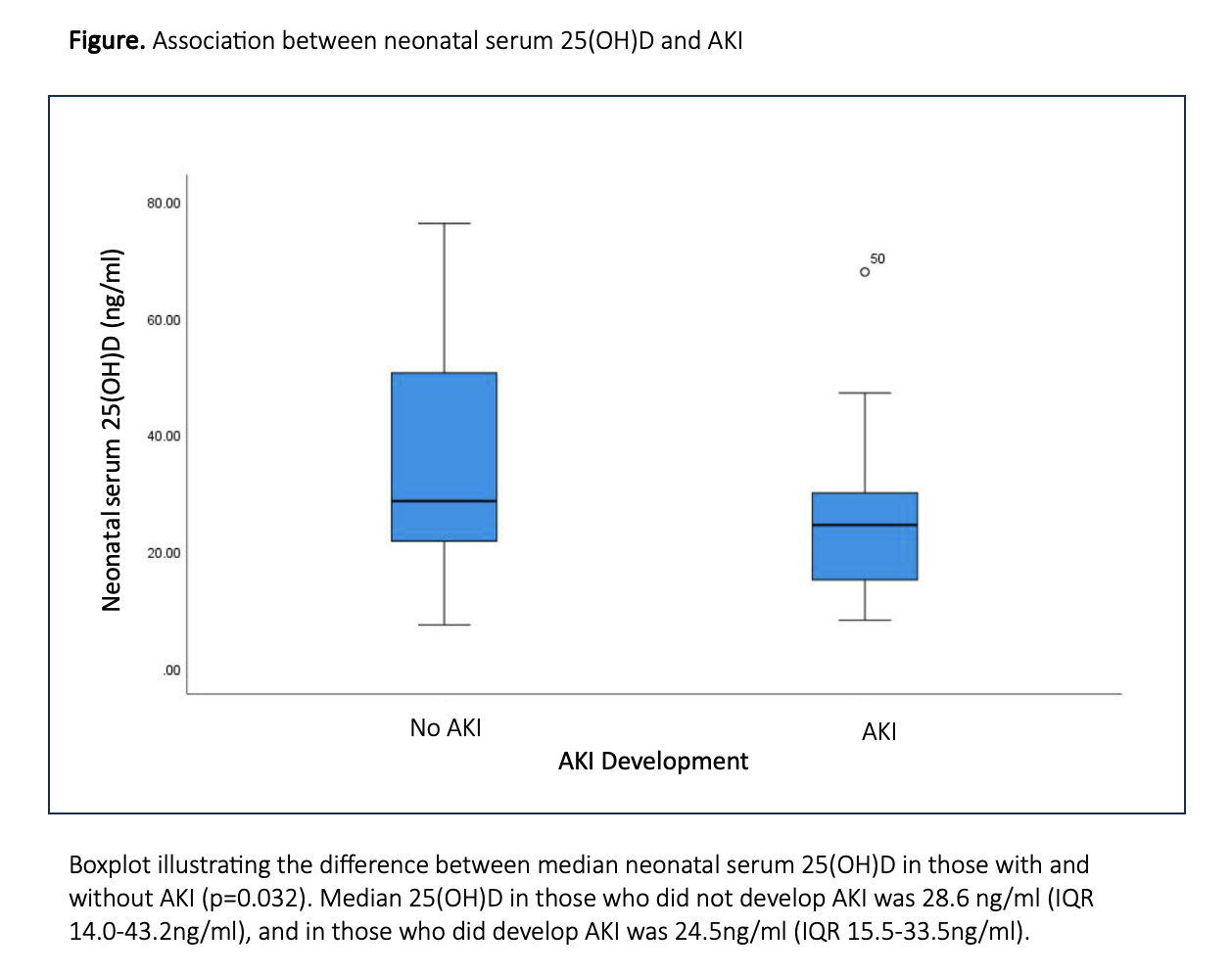
A significant association between serum 25(OH)D and neonatal AKI was detected (p=0.032, Table). The likelihood of VLBW neonates developing AKI during the first 90DOL was higher in those with lower serum 25(OH)D (p=0.04, Figure).
Conclusion(s): In this cohort of susceptible VLBW neonates during the first 90DOL, insufficient vitD status was associated with AKI (Figure). This finding emphasizes the importance of monitoring neonatal serum 25(OH)D and achieving adequate vitD status.
.png)