Neonatology
Session: Neo-Perinatal Health Care Delivery 1: Epidemiology/Health Services Research
314 - Contribution of Prematurity to Mortality in Congenital Diaphragmatic Hernia
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 314
Publication Number: 314.1499
Publication Number: 314.1499

Kuan-Chi Lai, MD, MPH
Assistant Professor of Clinical Pediatrics
Children's Hospital Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Mortality is high among neonates with congenital diaphragmatic hernia (CDH). Additionally, fetuses with CDH are at increased risk of preterm birth. However, the contribution of prematurity to mortality among infants with CDH is not known. The population attributable fraction (PAF) can be used to quantify how much prematurity contributes to mortality among infants with CDH at the population level.
Objective: To estimate the PAF of mortality attributable to prematurity among neonates with CDH.
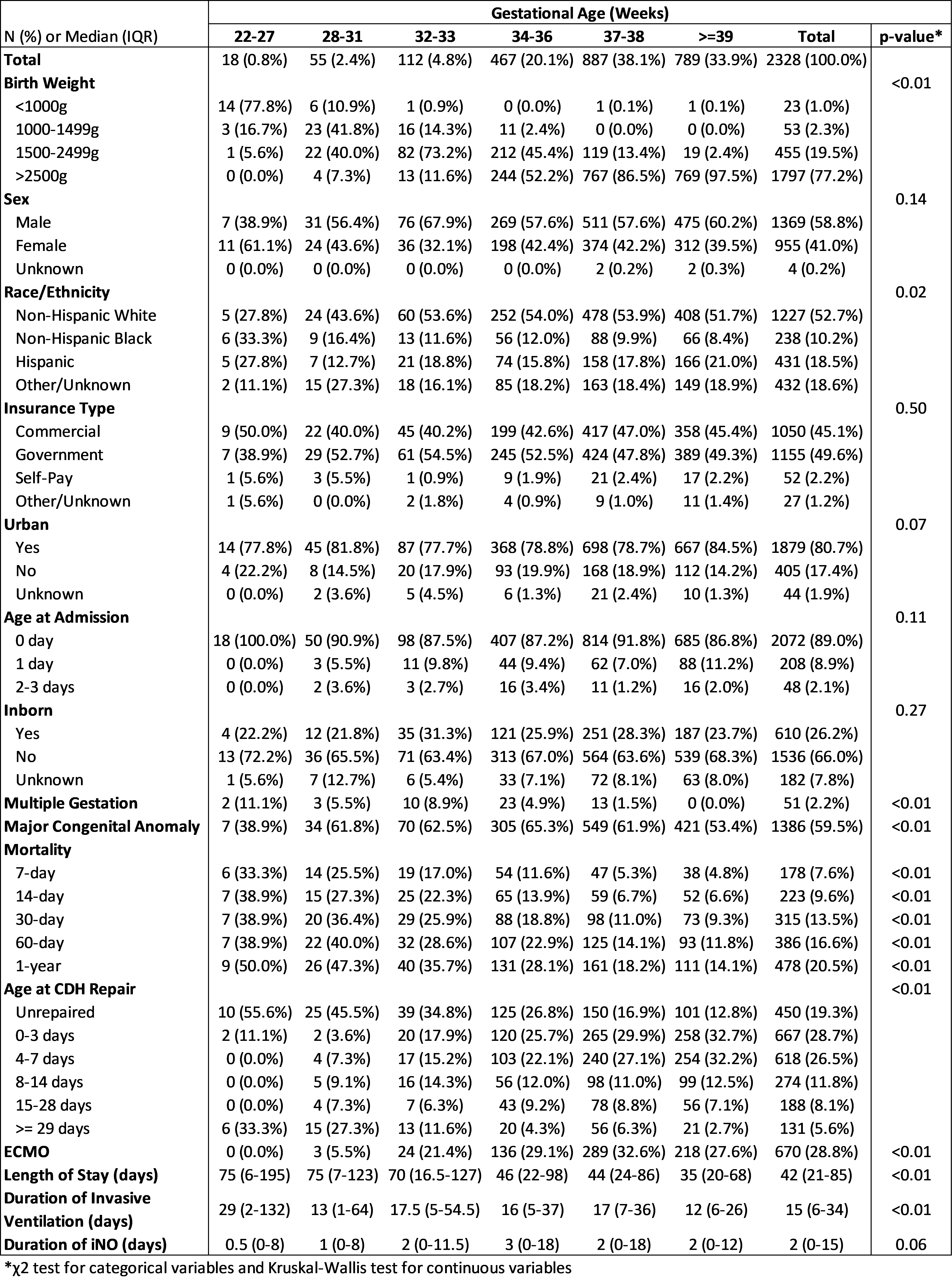
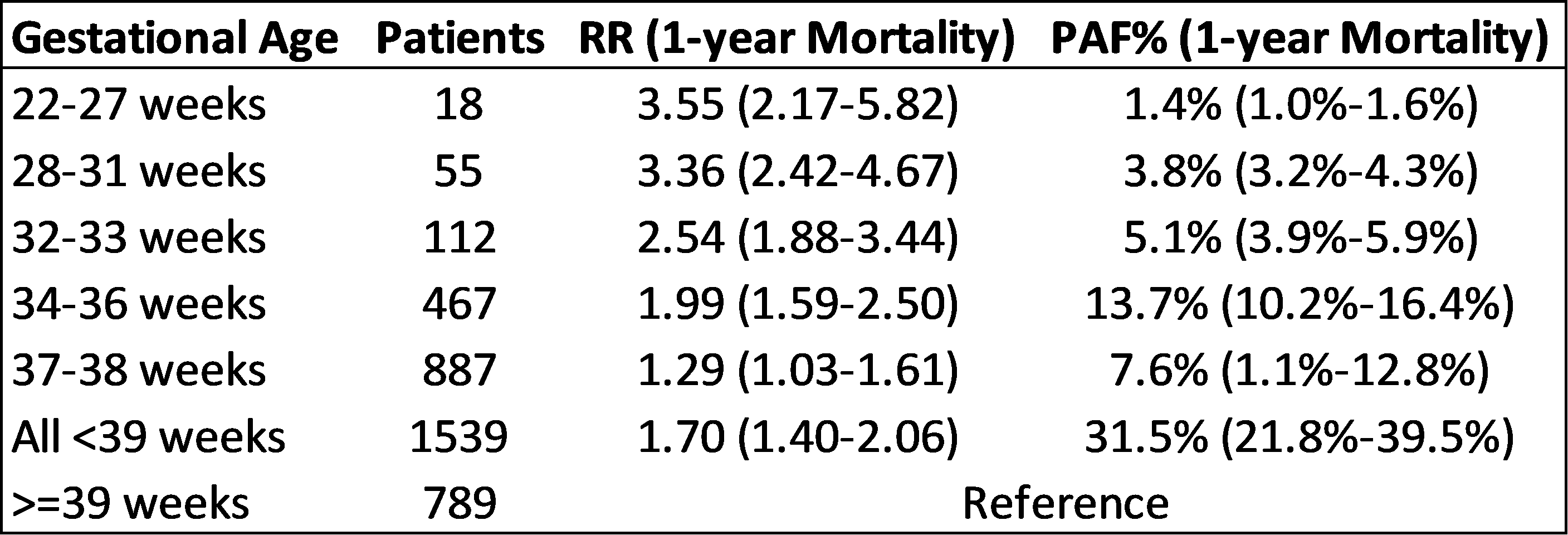
Design/Methods: Using the Pediatric Health Information System (PHIS), we conducted a retrospective cohort analysis of neonates born with CDH who were admitted to PHIS children’s hospitals within 3 days of life between 1/1/2016 to 12/31/2021. Patients were stratified by gestational age: extremely preterm (22-27 weeks), very preterm (28-31 weeks), moderately preterm (32-33 weeks), late preterm (34-36 weeks), early term (37-38 weeks), and full term (>=39 weeks). We used Poisson regression to estimate the relative risk (RR) of mortality in the first year of life for each prematurity age group vs full term, then calculated the PAF as Pr(preterm|mortality)(1-1/RR). To assess differential effects of patient characteristics on PAF, we performed stratified analyses of PAF of mortality due to prematurity within each patient characteristic strata.
Results: 2328 neonates with CDH (33.9% full term, 38.1% early term, and 28.0% preterm) were eligible (Table 1). Lower birth weight, non-Hispanic Black, multiple gestation, and major congenital anomalies were associated with prematurity. Among neonates with CDH, RR of mortality increases with lower gestational age as compared to full-term: RR = 1.29 [95% CI: 1.03-1.61] for early term vs. RR=3.55 [95% CI: 2.17-5.82] for extreme preterm (Table 2). The PAF of mortality attributable to prematurity for all preterm/early term ( < 39 weeks) when compared to full term (>=39 weeks) was 31.5% [95% CI: 21.8%-39.5%] with the largest PAF in the late preterm group (13.7% [95% CI: 10.2%-16.4%]). Stratified analyses (Figure 1) showed that prematurity had the largest PAF of mortality among those without additional major congenital anomalies (54.6% [95% CI: 39.7%-65.8%]).
Conclusion(s): Among neonates with CDH, risk of mortality increases with lower gestational age, and a significant proportion of mortality is attributable to prematurity at the population-level. This is especially true for late preterm infants. Efforts to safely extend gestation may decrease overall mortality among neonates with CDH and deserves further investigation.
.png)
