Medical Education
Session: Medical Education 4
396 - Leveraging Interprofessional Collaboration for Education: A Structured Conversation Guide for Pediatric Clerkship Students
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 396
Publication Number: 396.1502
Publication Number: 396.1502

Allison M. Fialkowski, MD (she/her/hers)
Resident Physician
Boston Children's Hospital
Brookline, Massachusetts, United States
Presenting Author(s)
Background: Interprofessional education (IPE) is endorsed by multiple professional and educational organizations, with an increasing emphasis on delivering IPE in authentic practice settings. Undergraduate medical educators are searching for effective models for delivering IPE during workplace learning.
Objective: This study explores how a structured conversation guide facilitated medical students’ 1) experience collaborating with other health professionals for patient care, 2) learning through joint reflection with those professionals about the collaboration, and 3) changes in their approach to future interprofessional interactions.
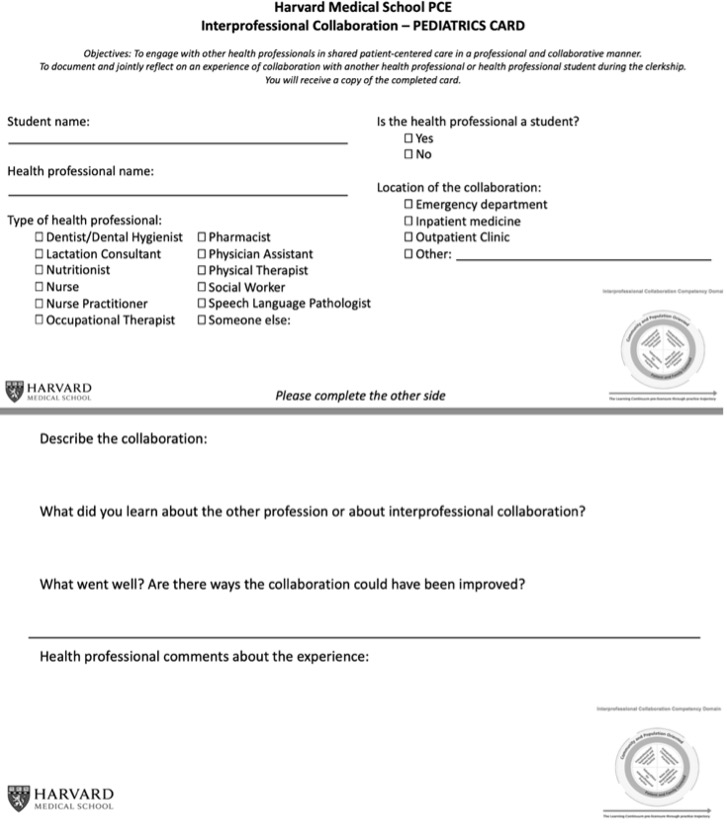
Design/Methods: We designed an Interprofessional Collaboration (IPC) Card (Figure 1) to facilitate a structured conversation around a patient care collaboration with an interprofessional colleague during the pediatric core clerkship at two hospitals during AY 2022-23. The card guided the conversation through three reflections completed by the student and one feedback prompt for the professional. We used a hybrid inductive-deductive approach to qualitative thematic analysis, sensitized by the Interprofessional Educational Collaborative competencies, to evaluate the activity using data from the written comments on cards and focus groups with students after the intervention.
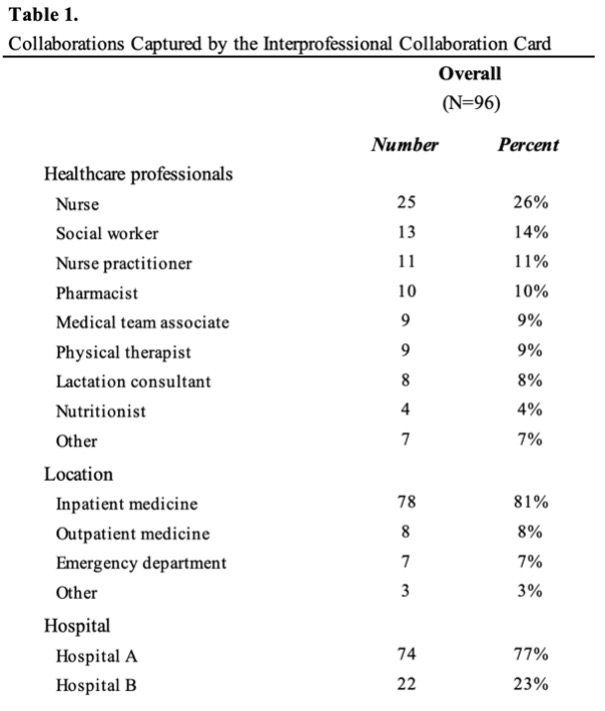
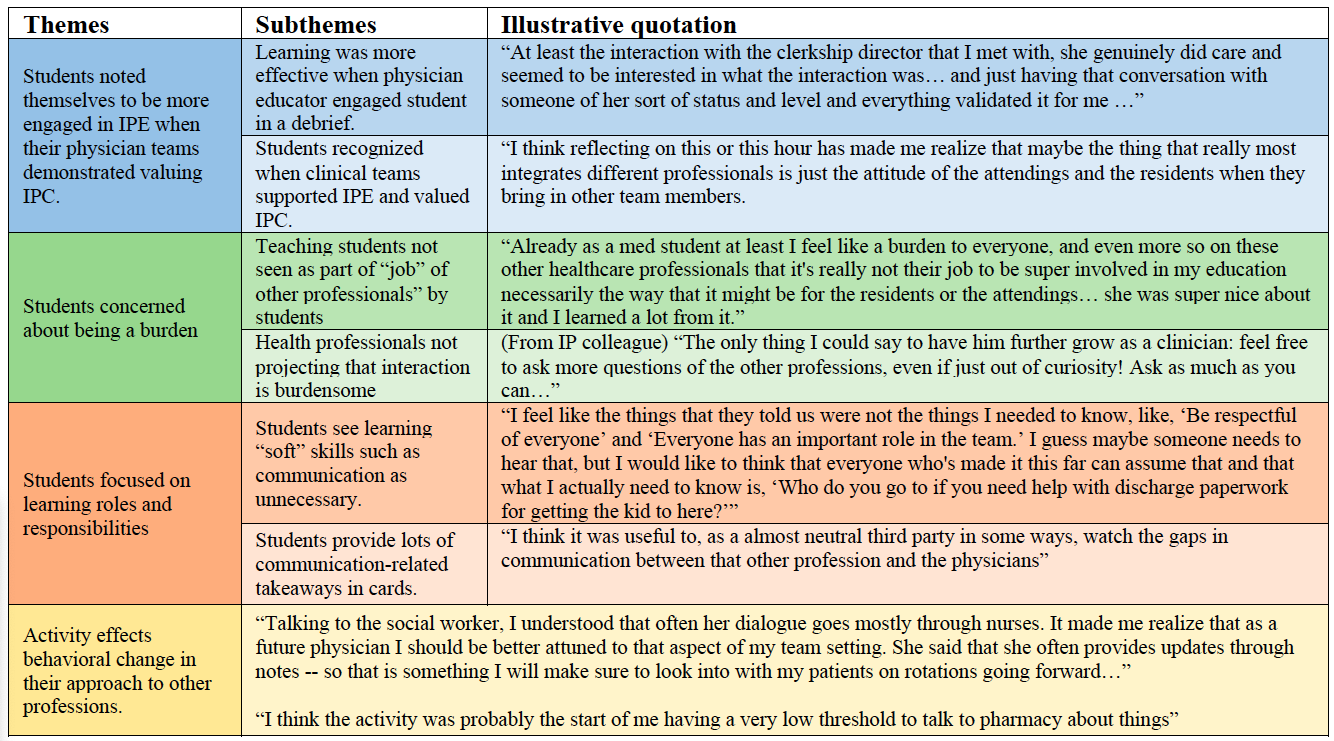
Results: Of 116 students, 96 (83%) submitted completed cards. We completed 4 focus groups (17 students). Students recorded collaborations with 14 different categories of professionals (Table 1). Four themes emerged in the qualitative analysis (Table 2). Students found the activity more valuable when their physician teams demonstrated valuing IPC and the assignment. Students expressed concern about their learning being a burden on other health professionals, while these professionals encouraged students’ curiosity. While students focused on learning roles and responsibilities and stated they possessed the requisite knowledge to collaborate, their written and verbal reflections expressed insights into communication and increased appreciation for the expertise of other professions. Students conveyed the assignment decreased their threshold to engage with other healthcare professionals and documented changes to how they would approach future IPC.
Conclusion(s): Our study affirms that the IPC Card can effectively facilitate IPE for medical students and guides actionable strategies for educators including: ensuring explicit support from physician teams, reducing the perceived burden on other healthcare professionals, and leveraging students’ focus on understanding roles and responsibilities to deliver other IPE objectives.