Neonatology
Session: Neonatal Hematology & Bilirubin Metabolism
455 - Late transfusions in the neonatal intensive care unit may be detrimental to neurodevelopmental outcomes
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 455
Publication Number: 455.1491
Publication Number: 455.1491

Kendell German, MD (she/her/hers)
Assistant Professor
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background: Red blood cell (RBC) transfusions are associated with adverse outcomes. Despite efforts to limit transfusions, most extremely preterm (EP) infants receive one or more RBC transfusions in the NICU.
Objective: To evaluate whether timing of RBC transfusions impacts neurodevelopment at 2 years corrected age (CA) among EP newborns.
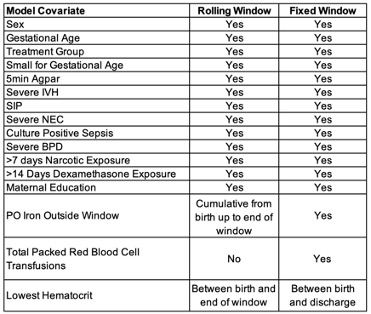
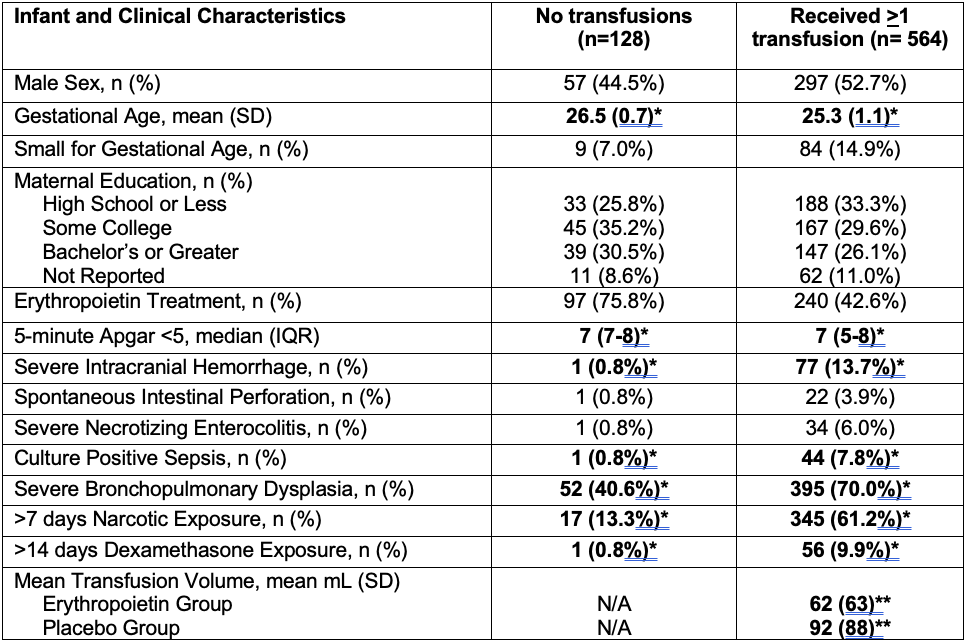
Design/Methods: This post-hoc analysis of the PENUT Trial data included infants born 24 0/7-27 6/7 weeks’ gestational age treated with erythropoietin (Epo) or placebo who completed 1 or more subscales of the Bayley Scales of Infant Development, 3rd edition (BSID-III) at 2 years CA. Correlation between BSID-III subscales and cumulative RBC transfusion volume in 3-week windows of postmenstrual age (PMA) were either rolling (RBC volume for each week plus the previous 2 weeks) or fixed (total RBC volume 27-29, 30-32, 33-35, 36-38, and 39-41 weeks’ PMA accounting for all other windows) in order to provide the best detail of the impacts at each PMA. Estimates were determined with 95% CI using generalized estimating equations accounting for clustering within siblings. All models were adjusted for confounders and predictors of long-term outcome (Table 1). Epo and placebo-treated infants were examined together; a sensitivity analysis was performed to evaluate effects of treatment assignment.
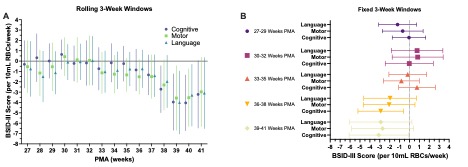
Results: 692 infants were included, 564 (83%) received at least one transfusion. Infant characteristics by transfusion exposure are summarized in Table 2. In rolling windows, there was no significant correlation between transfusion volume prior to 37 weeks’ PMA and any BSID-III subscale score. However, the relationship between transfusion volume and BSID-III scores appeared to worsen with advancing PMA at the time of transfusion (Fig 1). Total RBC volume was associated with significantly lower BSID-III cognitive scores for transfusions at 38-40 weeks PMA, and lower language and motor scores at 38 and 39 weeks PMA (Fig 1A). In fixed windows, RBC volume was associated with significantly lower cognitive scores in the 36-38 (-2.9; -5.2 to -0.6 points/10mL/week) and 39-41 (-3.1; -6.1 to -0.1 points/10mL/week) week windows (Fig 1B). There was no interaction between Epo and RBC volume on BSID-III subscales in any window (p>0.1).
Conclusion(s): This post-hoc analysis of EP infants demonstrates a negative correlation between RBC transfusion volume at later PMA and cognitive outcomes. Consideration of transfusion-limitation measures, particularly at later gestational ages, such as limiting phlebotomy, may improve long-term neurodevelopmental outcomes.