Neonatology
Session: Neonatal Quality Improvement 3
420 - Less is more! Standardized platelet transfusion practices in the NICU safely reduced prescribed transfusion volumes
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 420
Publication Number: 420.1876
Publication Number: 420.1876

Kristen Coletti, MD (she/her/hers)
Fellow
Childrens Hospital of Philadelphia
Wynnewood, Pennsylvania, United States
Presenting Author(s)
Background: Thrombocytopenia affects many neonatal intensive care unit (NICU) patients, including ~70% of extremely low birth weight infants. Platelets are transfused to thrombocytopenic patients to prevent bleeding, but current practices actually increase bleeding, respiratory morbidities and death. These findings may be explained by high transfusion volumes of 15mL/kg in infants. Prior studies demonstrate that 10mL/kg and 15mL/kg platelet transfusions equivalently treat thrombocytopenia.
Objective: We aimed to increase the percent of patients receiving a 10mL/kg platelet transfusion dose to 80% of ordered transfusions in our NICU. We hypothesized that 10mL/kg as compared to 15mL/kg platelet transfusions would minimize exposure to potentially harmful transfusion products without increasing transfusion frequency or bleeding complications.
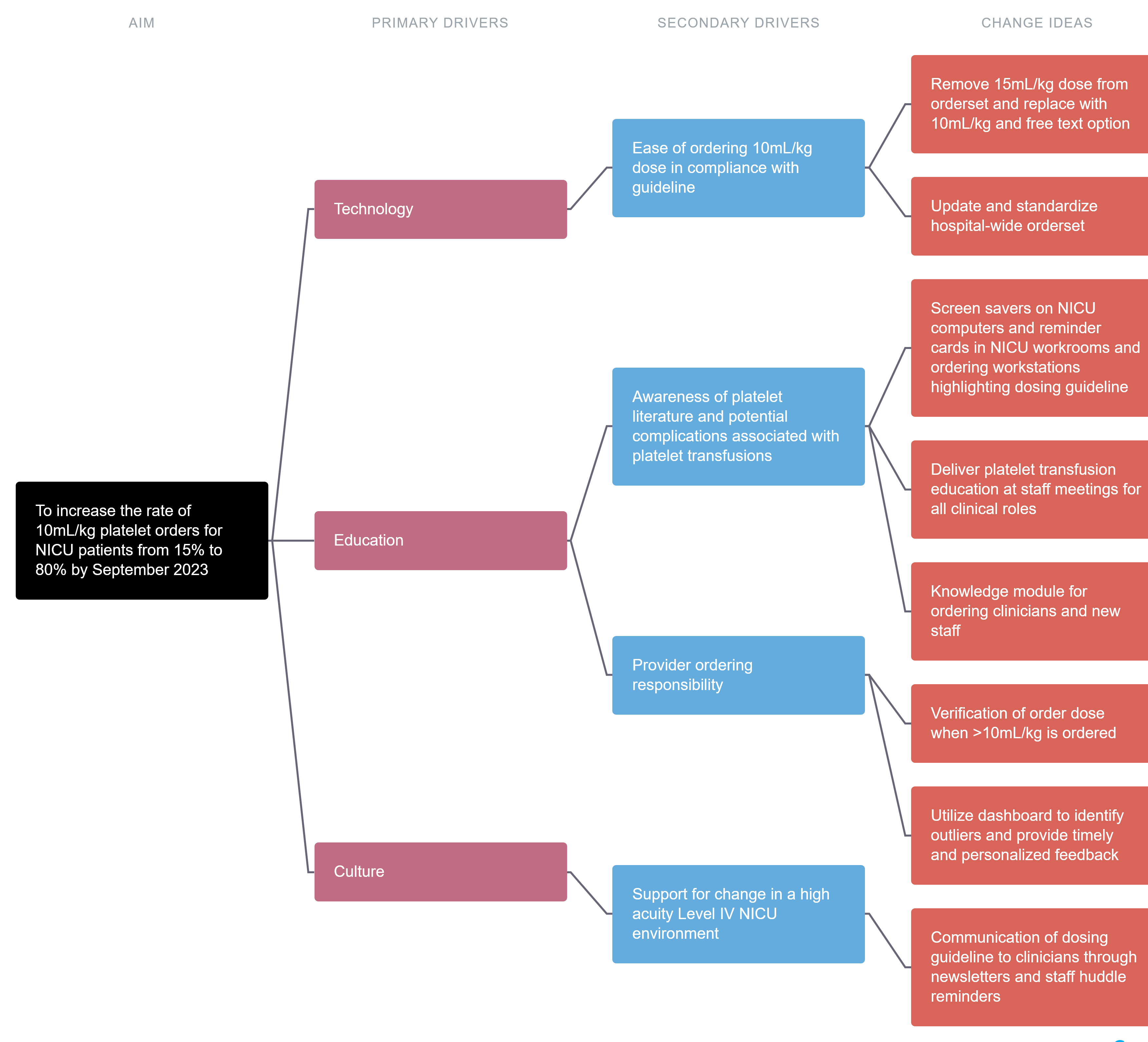
Design/Methods: A hospital-wide standardized prophylactic platelet transfusion dose of 10mL/kg was established through multidisciplinary collaboration. Drivers with interventions are listed in Figure 1. Infants with procedures/surgeries within 12 hours, on anticoagulation, bleeding, or on ECMO were excluded. The primary outcome measure was compliant platelet transfusions orders with a dose of 10mL/kg. We aimed for 80% compliance. Balancing measures included repeat platelet transfusions within 36 hours and clinical bleeding complications. Our initial two PDSA cycles focused on unit wide education and reinforcement of recommended dosing guidelines. The third PDSA cycle targeted unit technology, implementing clinical decision support changes to the medical record for ease of ordering the recommended dose. A graphic data display tool drawing from the electronic medical record was created to monitor platelet ordering in real time.
Results: We tracked 140 transfusions among 47 neonates. We surpassed our aim of 80% dosing compliance, noting special cause variation with sustained process change that resulted in a center line shift from 15% to 82% compliance (Figure 2). There was no change in the rate of subsequent platelet transfusions within 36 hours (Figure 3), nor an observed increase in bleeding complications.
Conclusion(s): We used clinician education and electronic medical record technology to standardize platelet transfusion practices within our NICU, reducing platelet exposure that has been linked with adverse outcomes in neonates.
.png)
.png)
