Newborn Care
Session: Newborn Care
219 - Improving Umbilical Cord Blood Gas Collection in Two Community Hospital Birth Centers: A Quality Improvement Initiative
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 219
Publication Number: 219.240
Publication Number: 219.240

Jennifer F. Konrad, FNP-BC (she/her/hers)
Clinical Nurse Specialist
Froedtert & Medical College of WI
Menomonee Falls, Wisconsin, United States
Presenting Author(s)
Background: The neonatal resuscitation team in community hospitals may have less experience in the critical components of post-resuscitation care, including the identification of newborns at risk for hypoxic-ischemic encephalopathy (HIE) by timely collection of umbilical cord blood gas (UCBG). Variations in practices due to the lack of national guidelines and universal UCBG determination may have further led to missed opportunities. We address these inconsistencies to optimize and standardize the care of newborns at risk for HIE across community hospital settings.
Objective: Increase the number of UCBG collected for newborns at risk for HIE and decrease the number of rejected UBCG specimens by 20% for a 6-month intervention period.
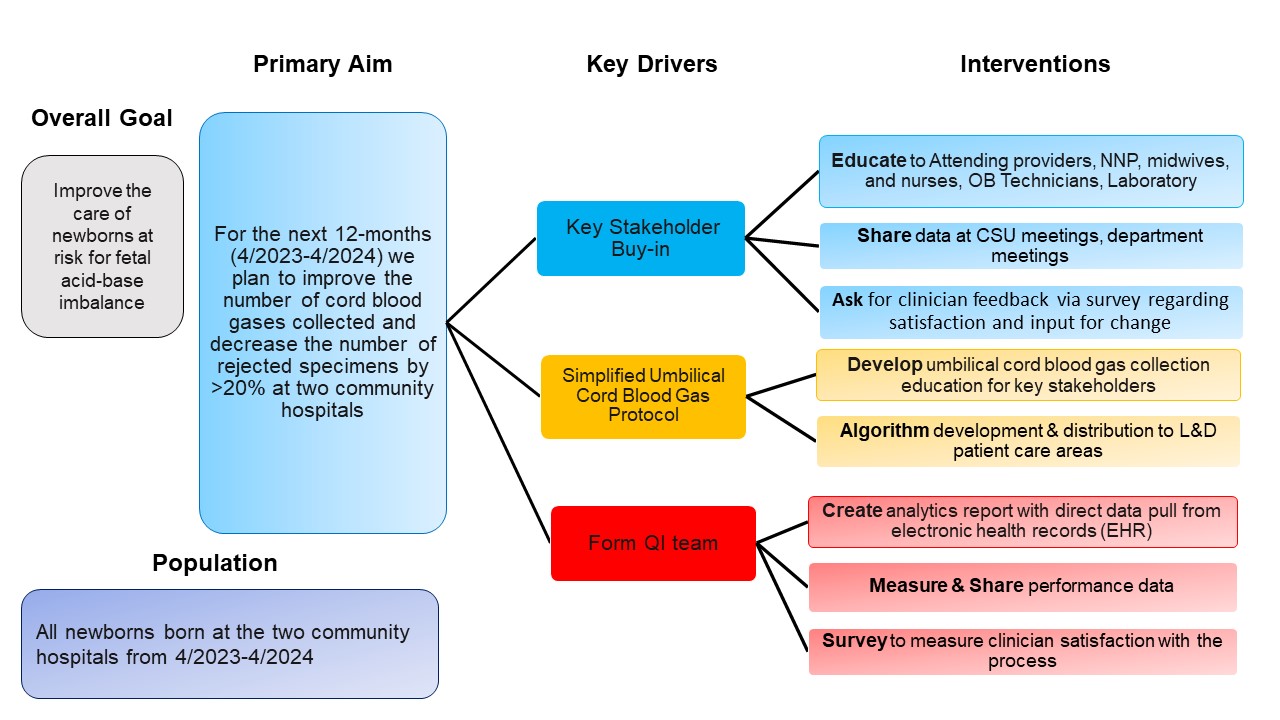
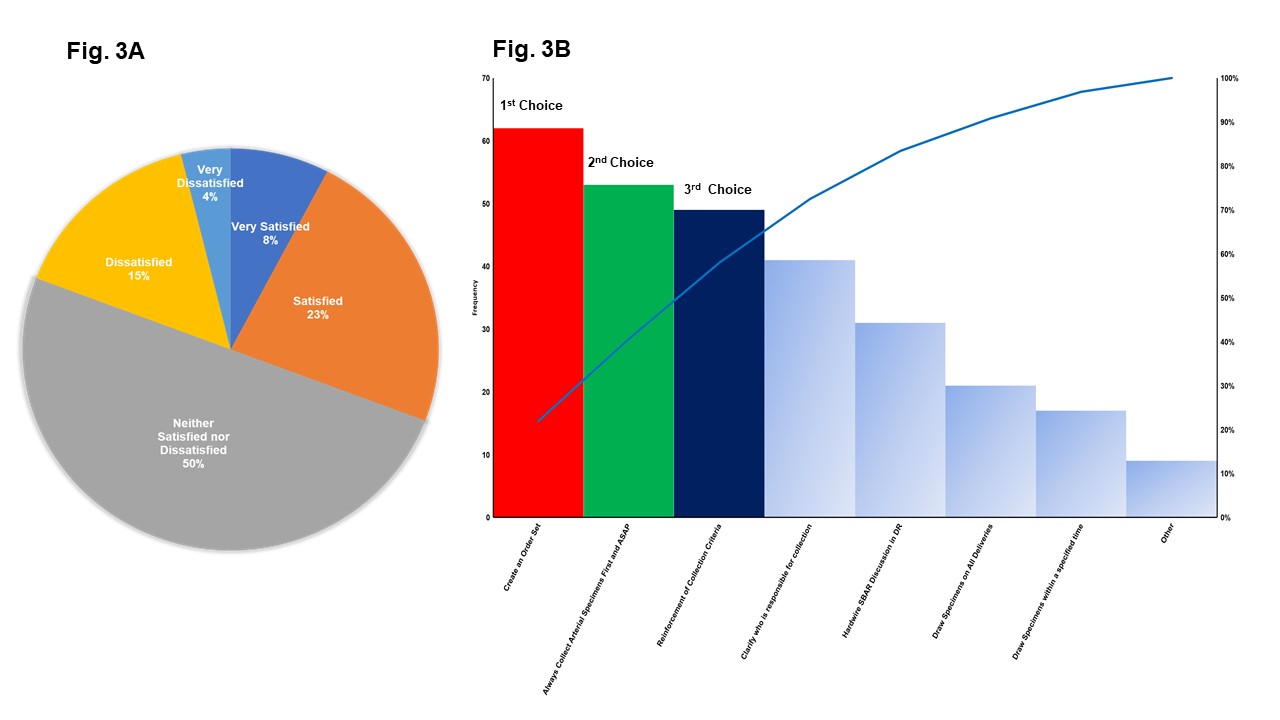
Design/Methods: This QI project was implemented at two community hospitals, building upon baseline data (7/22-3/23). This initiative had multiple plan-do-study-act (PDSA) cycles involving creating a multidisciplinary team. The team focused on key areas, including educating stakeholders on identifying at-risk newborns, timely and proper collection of UCBG, and developing and distributing UCBG algorithms (Fig. 1). Outcome measures included % increase in UCBG collected/total deliveries and specifically on newborns at risk for HIE. Process measures included % decrease in rejected UCBG specimens. On 7/22, a non-probability convenience sample survey was administered to stakeholders. The survey played two roles: balancing measure through assessing stakeholder QI satisfaction using a Likert scale; and their recommendations for improving UCBG collection. Statistical process charts were used.
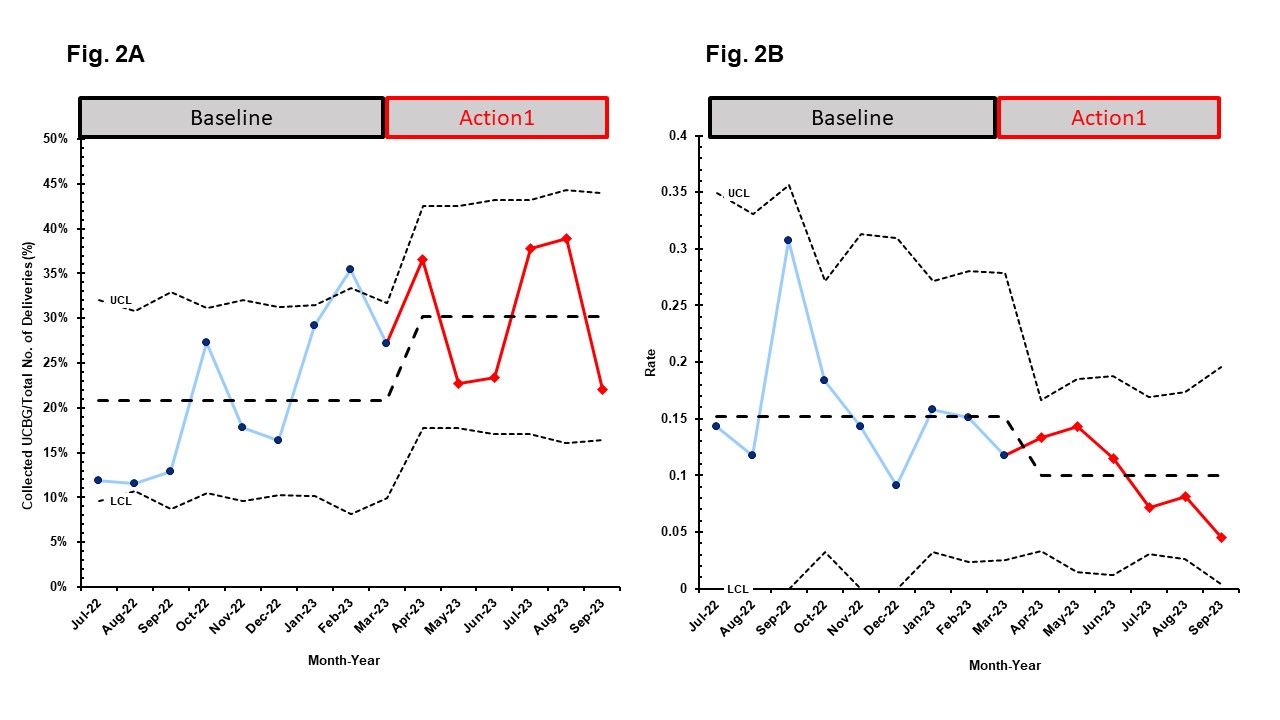
Results: For the 6-month period, we increased UCBG collection/total deliveries (mean = 20.8% to 30.3%), Fig. 2A, but UCBG collection/total at-risk for HIE newborns remained the same (58.5% to 57.0%). We decreased the rate of rejected samples per month (0.15 vs. 0.1), Fig. 2B. Additionally, there was a decline in the variability of the rejected samples. Out of the 53 stakeholders who participated in our survey, the majority were nurses (49%). Most participants were neither satisfied nor dissatisfied (50%) with the QI initiative (Fig. 3A). They called for an electronic health record (EHR) order set, prompt arterial UCBG collection, and reinforced UCBG collection criteria.
Conclusion(s): We increased overall UCBG collection rates but highlighted a need for focused improvement in UCBG collection for at-risk newborns. We reduced the rate of rejected samples, indicating enhanced consistency in our practices. Next steps include implementing the stakeholder feedback recommendations.