Neonatology
Session: Neo-Perinatal Health Care Delivery 3: Epidemiology/Health Services Research
258 - Experiences of Communication in the Neonatal Intensive Care Unit for Mothers with Preferred Language Other than English
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 258
Publication Number: 258.1892
Publication Number: 258.1892

Nikita S. Kalluri, MD (she/her/hers)
Neonatal-PerinatalMedicine Fellow
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Emerging data has shown that mothers and families with a preferred language other than English (PLOE) have lower participation in family-centered care behaviors (e.g. kangaroo care) and increased rates of neonatal intensive care unit (NICU) morbidities compared to those that speak English. The experiences of mothers with PLOE surrounding staff communication and engagement that may contribute to these findings are unknown in the complex NICU environment.
Objective: To understand the lived experience of mothers with PLOE in communicating with hospital staff and engaging in care of their infant(s) hospitalized in a NICU.
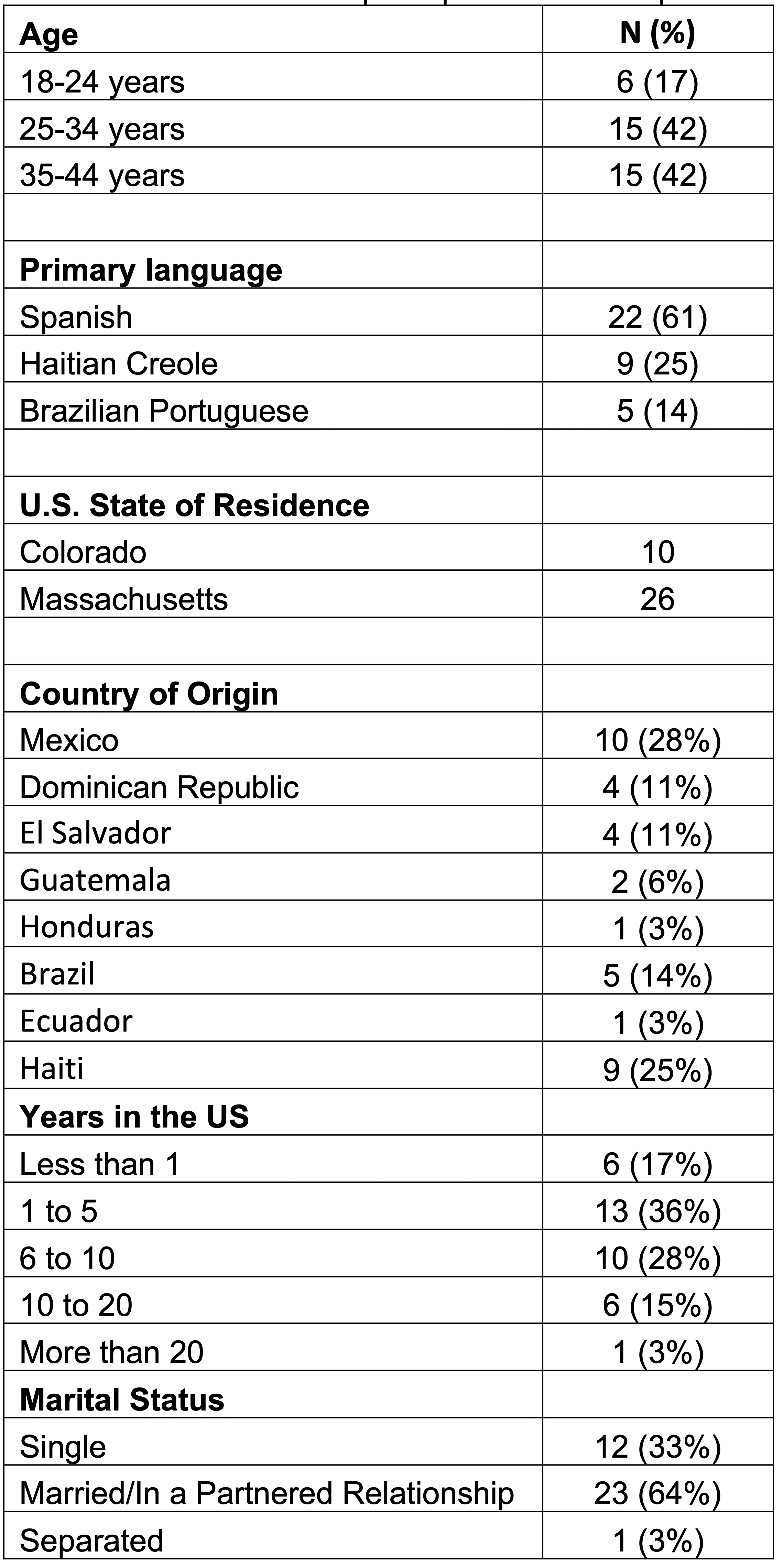
Design/Methods: We leveraged existing qualitative interviews conducted 2-6 months post-discharge of 30 in-depth Spanish- and Haitian Creole-speaking mothers of preterm infants. These interviews were performed to evaluate experiences of engagement in NICU care and discharge teaching. We prospectively performed 6 interviews with Brazilian-Portuguese speaking mothers prior to NICU discharge. All interviews probed about the role of mothers’ PLOE in their perceptions of support and engagement in NICU care. We used the constant comparative method to select important concepts and to develop codes and themes. We inductively determined to use the socio-ecological framework (SEM; individual, interpersonal, and institutional) to group themes for presentation.
Results: Characteristics of mothers are shown in Table 1 and themes and quotes are shown in Table 2. Unaddressed barriers to communication negatively impacted maternal engagement in NICU care across all SEM levels. At the individual level, mothers felt varied degrees of empowerment to request an interpreter and many justified suboptimal interpreter use by the clinical team. At the interpersonal level, mothers identified language concordance of hospital staff as a strong facilitator for engagement and highlighted the positive impact of non-interpreted informal interactions on communication. However, mothers recognized differential treatment based on staff-mother language concordance. Institutionally, there were system-level barriers to interpreter access and varied quality of interpreter services.
Conclusion(s): Findings indicate that there are multilevel barriers to the experience of NICU communication and engagement for mothers with PLOE. Language-specific NICU interventions, such as language & culturally concordant staff, consistent interpreter access and quality, multilingual educational materials, and empowerment of mothers may represent targets to improve disparities in NICU engagement.
PASQuoteTable.jpeg
