General Pediatrics
Session: General Pediatrics 1
234 - Text Outreach Promotes Adolescent Tobacco Cessation: Results from a Clinical Workflow Pilot
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 234
Publication Number: 234.245
Publication Number: 234.245

Gabrielle DiFiore, MPH (she/her/hers)
Clinical Research Project Manager
Children's Hospital of Philadephia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Almost all adult tobacco use starts during adolescence. Despite many adolescents tobacco users reporting wanting to quit, few adolescents engage in treatment. Few studies examine the effectiveness of behavioral or pharmacotherapy interventions in adolescents, largely driven by challenges with enrollment, adherence, and retention of adolescents. New methods are needed to identify adolescents who use tobacco and engage them in treatment.
Objective: Through a single-armed pilot study in a large primary care network, evaluate the use of screening for adolescent tobacco use and desire to quit through routine pediatric care combined with after-visit text-message treatment navigation on rates of treatment acceptance.
Design/Methods: Adolescents aged 13-18 years seen for a preventative visit from February-May 2023 completed a standardized health behavior screener, the Adolescent Health Questionnaire (AHQ). The AHQ screened for tobacco/nicotine use in the past 30 days and interest in learning more about tobacco treatment options. Adolescents who expressed interest in quitting were contacted by a health navigator, via text, and offered 3 treatment options: counseling via text (This is Quitting), counseling via phone (My Life, My Quit), and/or nicotine replacement therapy (NRT). Adolescents interested in NRT were connected to a pediatrician via phone to assess nicotine severity, prescribe NRT, and review appropriate use. We measured interest in quitting, engagement with the navigator, and treatment acceptance.
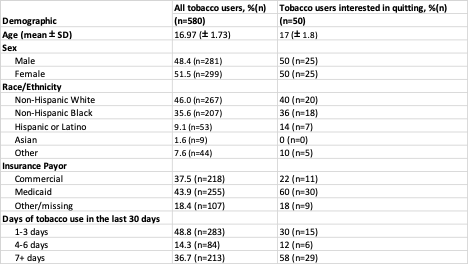
Results: Of 16,207 adolescents who completed the AHQ during the pilot period, 4% (n=580) reported tobacco use. Of those, 9% (n=50) expressed interest in quitting (Table 1). The health navigator texted 34 patients (16 were ineligible due to language barriers, no personal phone number, or inaccurate responses), 12 of whom responded and were still interested in quitting. Of those, 6 accepted the This is Quitting program and 6 engaged in a phone conversation and were prescribed NRT (Figure 1).
Conclusion(s): This pilot demonstrates that while there is likely underreporting of tobacco use and interest in quitting among adoelscents in pediatric primary care, text messaging may hold potential as an effective mode of engagement and treatment referral for those interested in quitting. Of the 50 adolescents interested in quitting, 12 (24%) were connected to evidence-based treatment. Further work is needed to support adolescent tobacco use disclosure and treatment engagement.
.png)