Hospital Medicine
Session: Hospital Medicine 3
329 - “Tea Time Teaching”: A low-cost strategy for interdisciplinary skill building by community pediatric hospitalists
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 329
Publication Number: 329.246
Publication Number: 329.246

Sara Szkola, MD (she/her/hers)
Clinical Assistant Professor of Pediatrics
Stanford University School of Medicine
Greenbrae, California, United States
Presenting Author(s)
Background: Since 2008, an estimated 18.4% of pediatric units within general hospitals have closed. The remaining community pediatric units often must provide care for complex patients with more limited staffing and resources compared to university-based settings. In this setting of resource reduction, community pediatric hospitalists have an opportunity to improve the skill set of the interdisciplinary neonatal and pediatric team.
Objective: 1. Describe a novel, low-cost program to increase confidence and competence in neonatal skills in an interdisciplinary team
2. Explore participants’ perceived skill level before and after completion of the program, and their feedback about the program.
Design/Methods: From May to October 2023, a pediatric hospitalist regularly engaged staff on a joint maternal-child unit in 1 minute “Tea Time Teaching” sessions at a single community hospital during a pre-scheduled “Safety Huddle.” The physician taught one skill (appropriate neonatal face mask selection for positive pressure ventilation and appropriate implementation of hyperbilirubinemia guidelines) at each session, and repeated the teaching an average of 4x/month over the course of 3 months. Participants completed an anonymous pre and post survey with a modified 5-point Likert scale asking about their confidence performing a skill and general feedback about the session. Responses were analyzed using descriptive statistics.
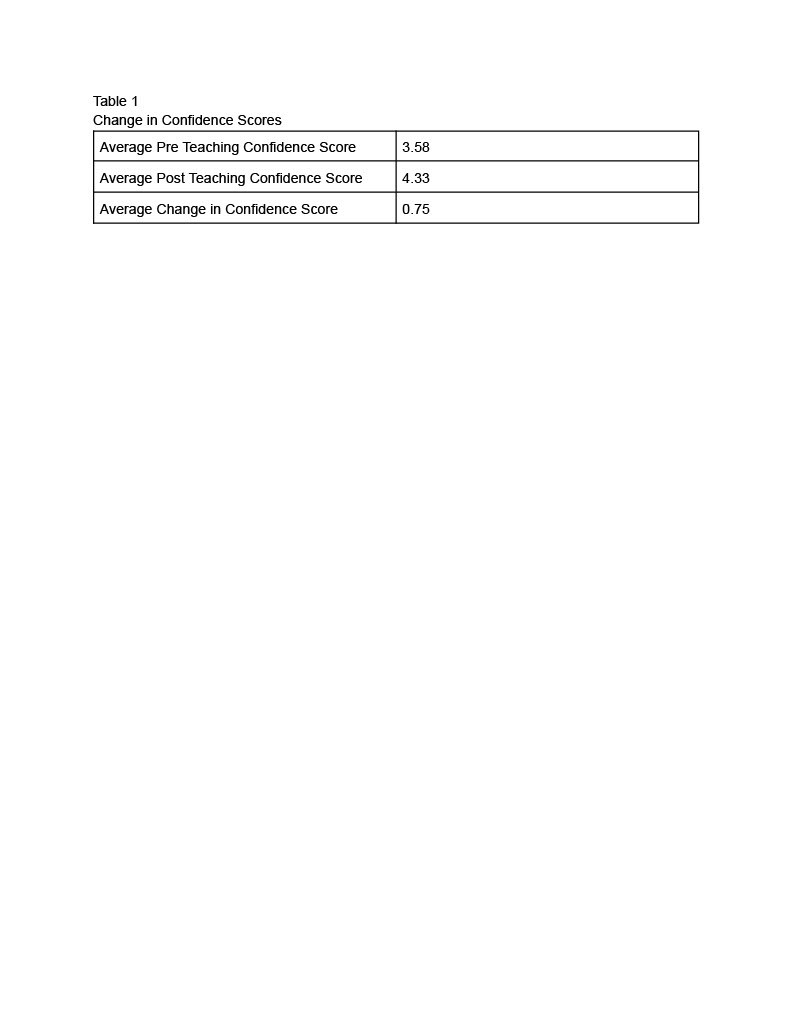
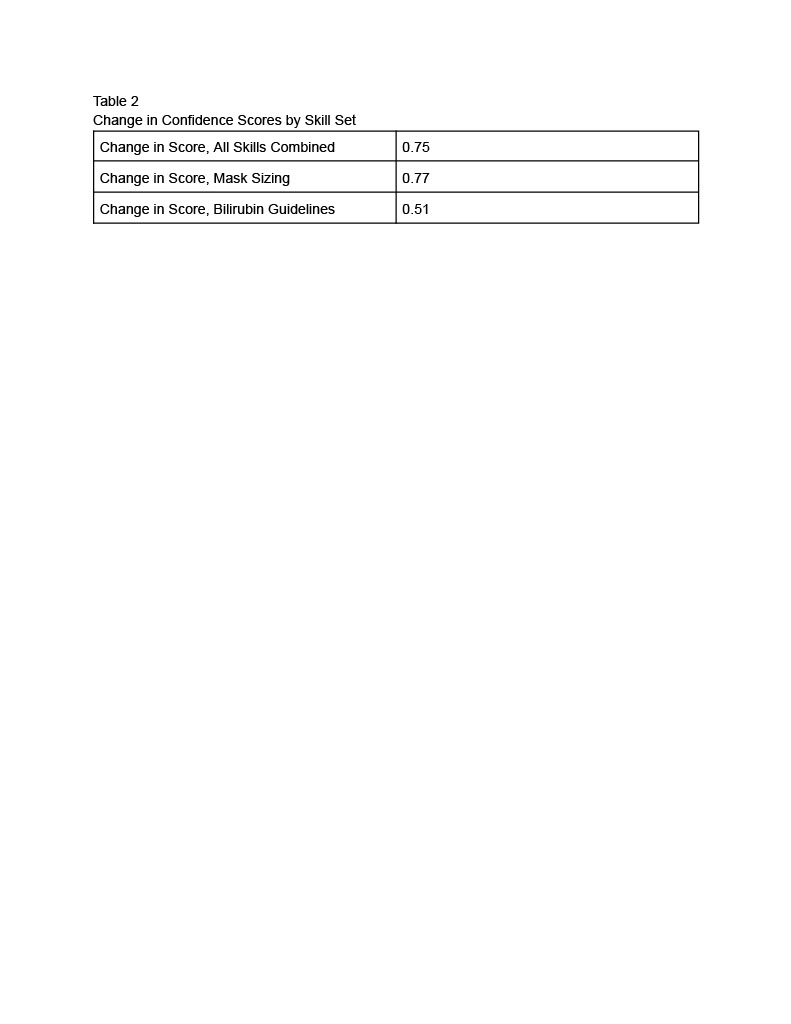
Results: 52 of 52 program participants completed the pre/post survey. 88.5% of participants were RNs, 2% were MDs, and 9.5% were other staff. Overall, there was a mean improvement of self-rated confidence in the skills being taught of 0.75 (range 0-3). For choosing the appropriate sized face mask, the mean improvement was 0.77 (N=30). For appropriate implementation of hyperbilirubinemia guidelines, the mean improvement was 0.51 (N=22). Themes in the open-ended feedback included importance of verbal/auditory learning cues, requests for more frequent teaching, and a suggestion to mandate the training for all patient care staff.
Conclusion(s): Community pediatric hospitalists can play a critical role in building core care and resuscitation skills among staff members. “Tea Time Teaching” is a low-cost, time-efficient endeavor that can bolster ancillary staff skills and increase the capacity of community hospitals to care for ill children. More research is needed to further evaluate this method across settings and institutions.