Medical Education
Session: Medical Education 9
498 - 3D Printing to Maximize Medical Simulation Training in Neonates: A Unique Collaboration with the Department of Defense
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 498
Publication Number: 498.3123
Publication Number: 498.3123

Daniel Scheese, MD
General Surgery Resident
Virginia Commonwealth University School of Medicine
Richmond, Virginia, United States
Presenting Author(s)
Background: The Department of Defense (DOD) and Department of Neonatology collaborated to design a 3D printed (3DP) umbilical cord catheterization (UCC) task trainer with a higher degree of realism and a lower cost than current market models. 3DP technology has emerged as a promising approach to develop highly customizable models that can transform the medical educational experience. Medical scenarios characterized by high acuity but low occurrence carry significant repercussions for the overall survival of patients. In neonatal resuscitation, emergent UCC is a critical procedure performed by Neonatal Resuscitation Program (NRP) certified providers. Reported statistics indicate that less than 1% of live births will require this procedure, and the retention of skills acquired in certification courses only lasts 6-12 months. UCC simulation practice is essential in emergency preparedness to care for newborn patients. Utilizing 3DP simulation models allows for quick iterative changes, at a fraction of the cost of market models.
Objective: Use of 3DP UCC task trainer in NRP training to improve medical provider competency, therefore improving patient outcomes from neonatal resuscitation.
Design/Methods: The DOD developed an initial 3DP UCC model. Experienced provider feedback from neonatology faculty guided size and material iterative changes, creating a 2nd model. IRB approval was obtained to allow for incorporating and evaluating the use of the 3DP UCC models into respective training programs. Between 9/2022–10/2023, both models were employed in training of medical providers. A feedback survey was administered to trainees which included: vessel attributes, ease in cannulation, and trainee UCC skill competency prior to and after simulation.
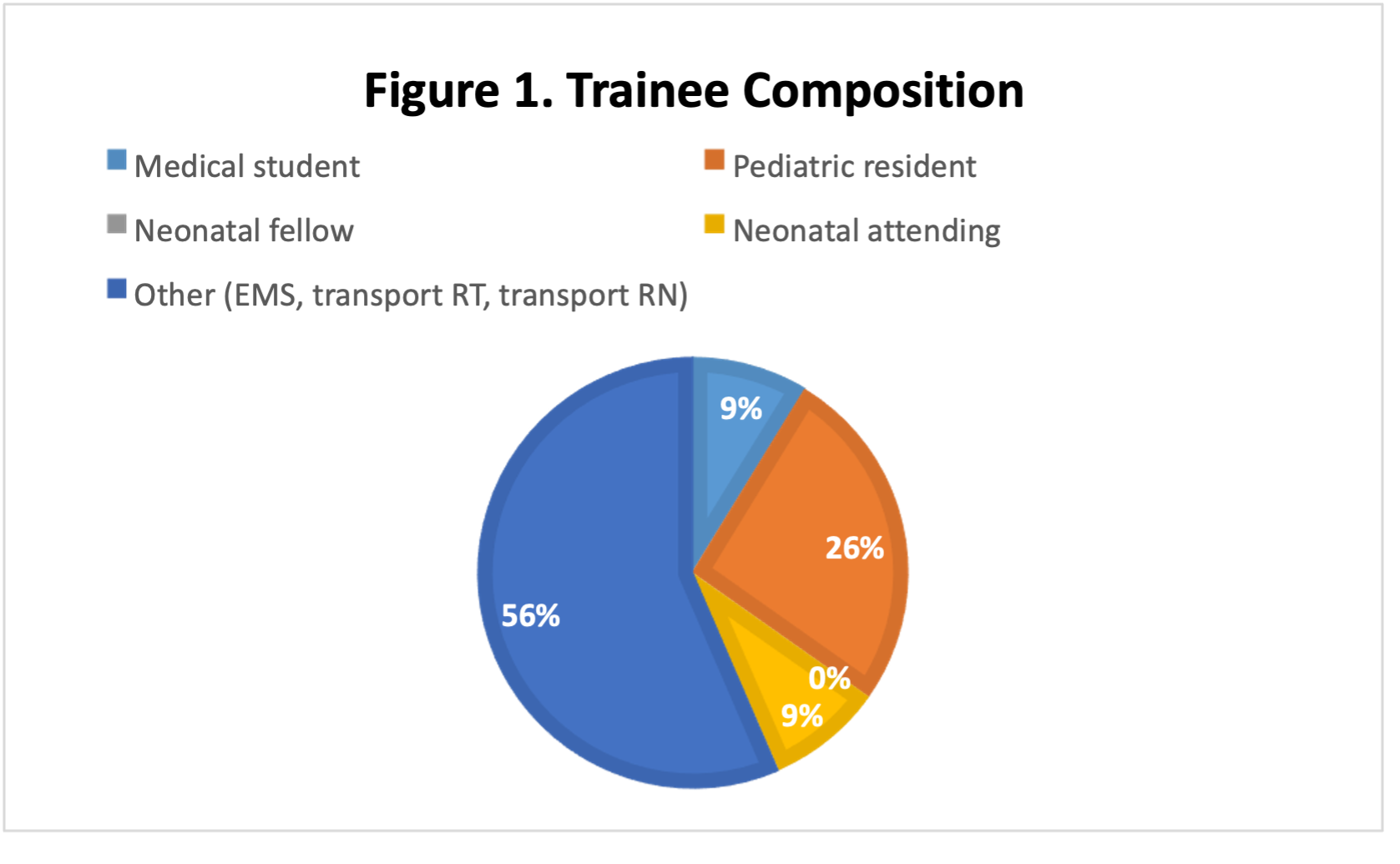
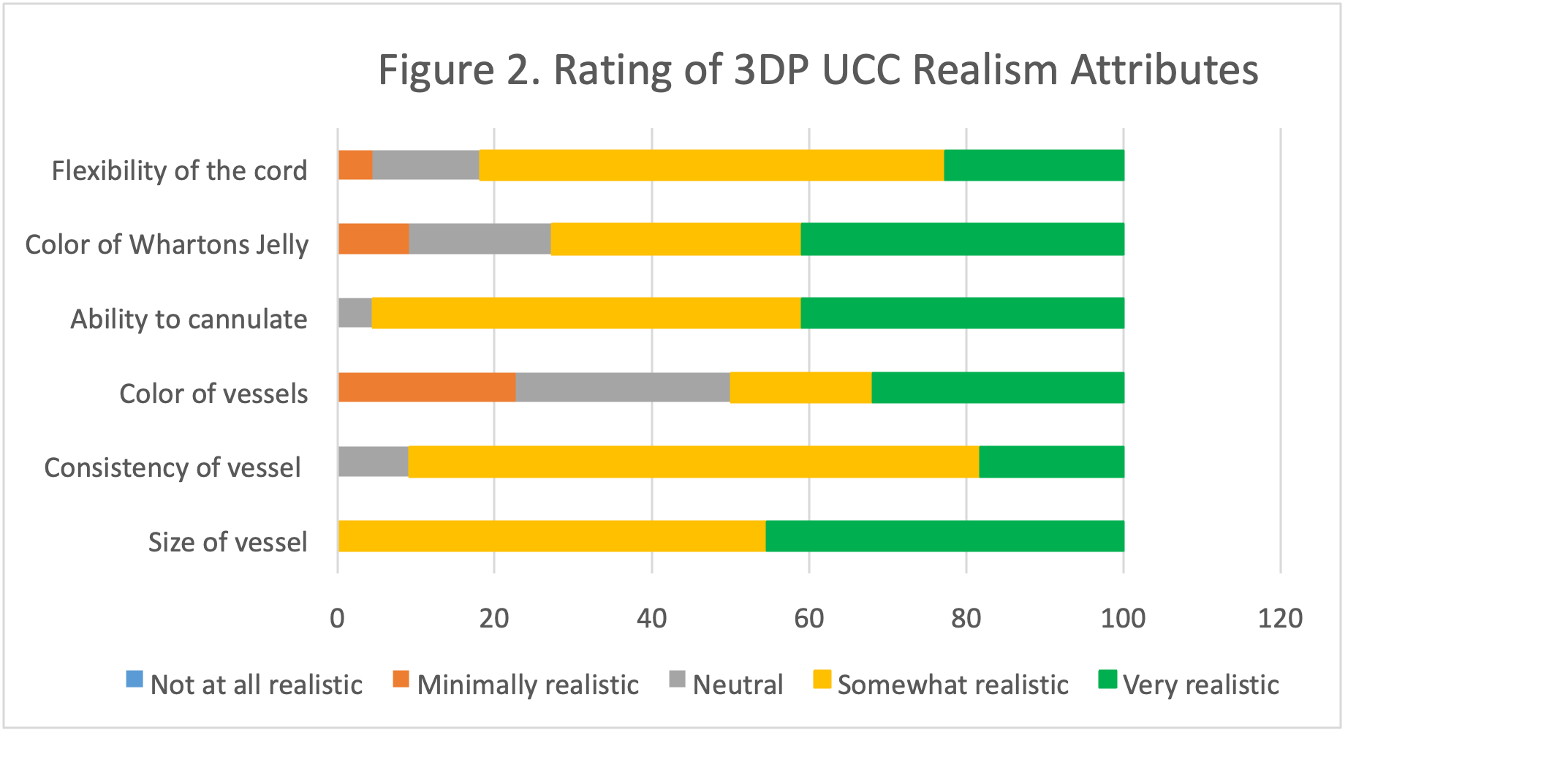
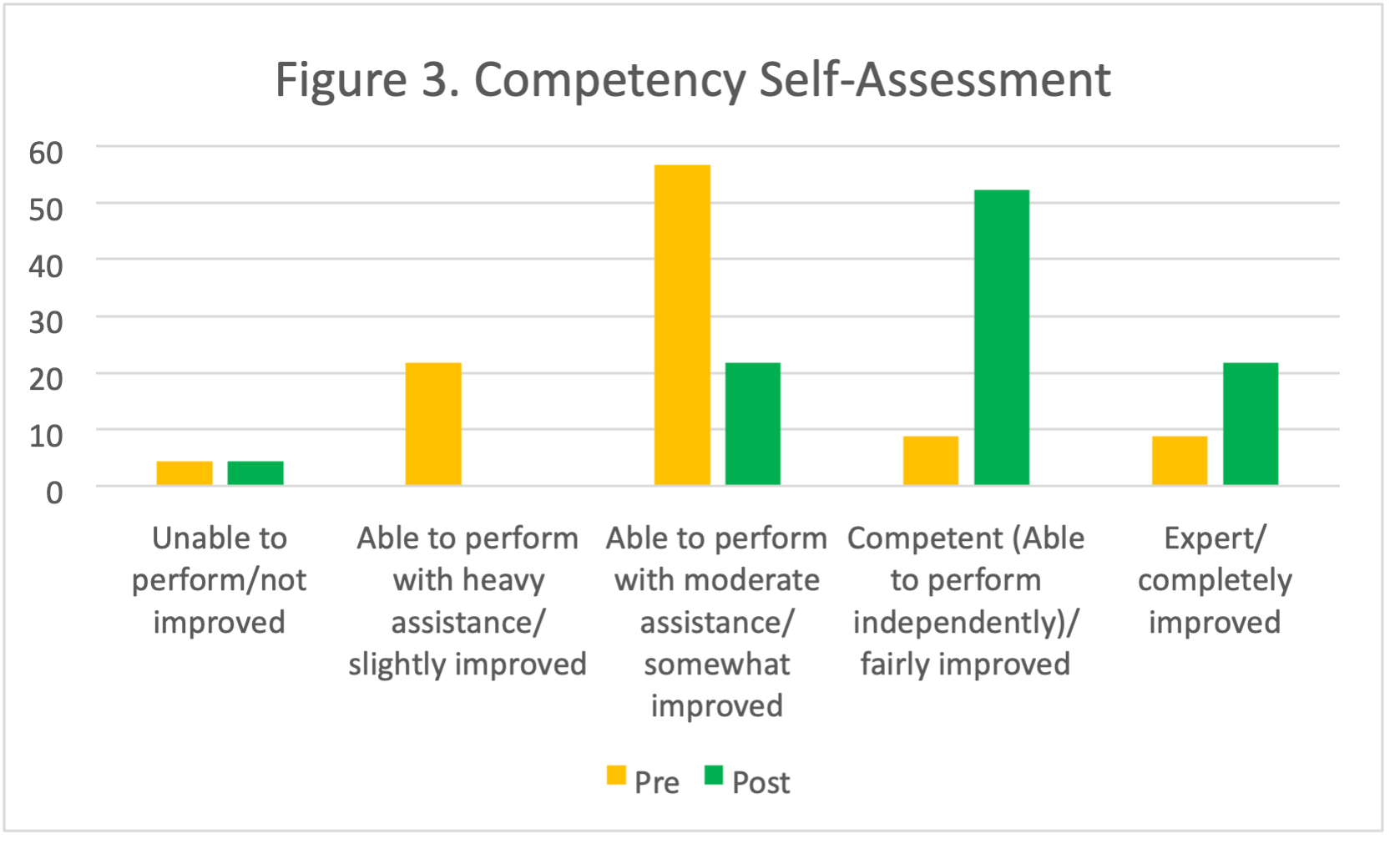
Results: 23 trainees used the 3DP UCC task trainer and completed the survey. The composition of trainees are in figure 1. 91% of trainees had prior experience performing the procedure. The 3DP UCC model was rated on realistic attributes (figure 2). This demonstrates variation in physical characteristics and size expectations can be variable based on provider experience and preferences. Pre and Post training competency self-assessment was completed (figure 3). 94% of our trainees valued the application of 3D printing in medical training.
Conclusion(s): Our collaboration between the DOD and Neonatology department has resulted in the development of a highly realistic and cost-effective 3DP UCC task trainer. This innovative approach to medical education offers the potential to enhance the competency of medical providers, ultimately improving patient outcomes in neonatal resuscitation.