Children with Chronic Conditions
Session: Children with Chronic Conditions 1
258 - Days at Home: Experiences of Caregivers of Children with Medical Complexity
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 258
Publication Number: 258.261
Publication Number: 258.261

Claire Washabaugh, BS (she/her/hers)
MS4
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background: Children with medical complexity (CMC) have frequent healthcare encounters that keep them and their families away from home and usual daily activities. Days at home (DAH) – defined as days without healthcare visits – has been proposed as a patient-centered outcome measure of health service use and care coordination. The value of DAH as an outcome rests on the assumption that days spent at home are inherently good and that more DAH are better for patients/families. However, it remains unclear whether this assumption is supported by the perspectives of parents/caregivers of CMC.
Objective: To describe perspectives of parents/caregivers of CMC on “good days at home.”
Design/Methods: This is a community-engaged, qualitative descriptive study. Our community partner, a statewide family advocacy organization, was centrally involved in study design and recruitment. To ensure informational representation from a range of context-dependent experiences, we used purposive sampling to recruit parents/caregivers of CMC who have recently experienced ‘missed days of school/work’ and ‘disrupted days at home’. Eligible parents participated in a virtual (Zoom) 60-minute semi-structured 1:1 qualitative interview which was recorded and transcribed. We analyzed and coded each transcript to explore key themes, with the Healthy Life Domains of CMC serving as an a priori analytical framework.
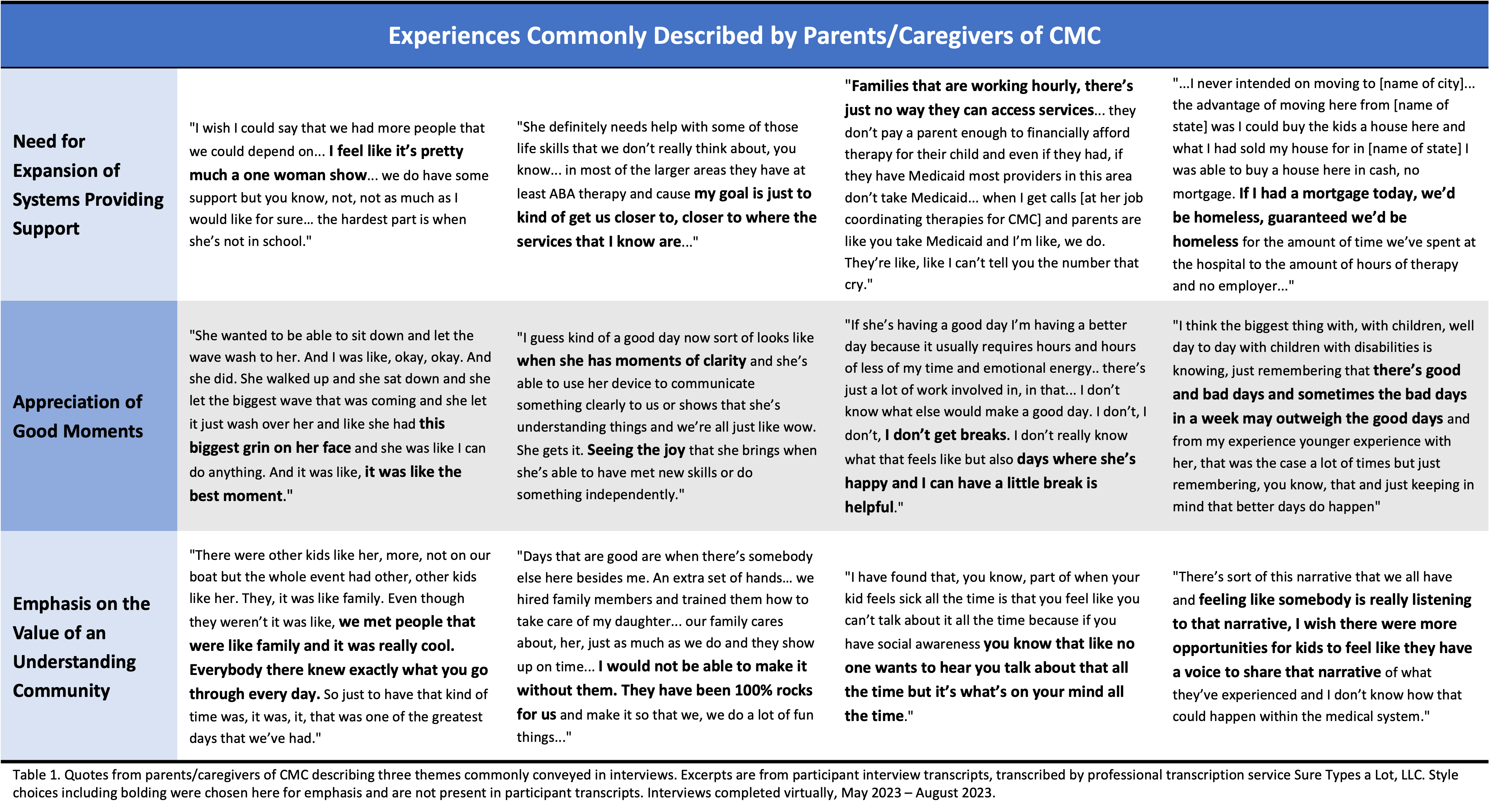
Results: Analyses completed for 8 of 17 (47%) interviews represent preliminary themes. DAH were consistently reported as challenging. Experiences of DAH varied by home- and community-based supports. Families with shared caregiving support from an accessible social network and/or home-based clinical services generally described more hopeful perspectives, while those with limited caregiving support often expressed feelings of isolation and defeat. Notably, common experiences transcended these archetypes, including a need for expansion of systems providing support (particularly for school/education, financial costs of therapies, and access to therapies), an appreciation of good moments, and an emphasis on the value of a community that understands the demands and needs of caregiving (Table 1).
Conclusion(s): Parents/caregivers CMC reported that DAH are challenging and that not all DAH are inherently ‘good.’ Parents emphatically recommended greater system-level support to improve DAH for CMC and their families. While measures of DAH reflect healthcare utilization, quantitative measure of DAH as a family-centered outcome should integrate perspectives of parents/caregivers to ensure the measure best reflects their lived experiences.