Children with Chronic Conditions
Session: Children with Chronic Conditions 2
275 - Indications and Outcomes of High Flow Nasal Cannula in the Home Setting among Children and Youth
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 275
Publication Number: 275.270
Publication Number: 275.270

Liam Sanvido
Medical Student
University of Ottawa Faculty of Medicine
Vaughan, Ontario, Canada
Presenting Author(s)
Background: High-flow nasal cannula (HFNC) has commonly been used in the inpatient and intensive care setting for children with acute respiratory distress. Recently, HFNC has been applied in the home setting for a variety of conditions. The novelty of home HFNC use and an absence of clear indications contribute to wide practice variability in the application of home HFNC.
Objective: We aim to describe the patient characteristics, indications, and clinical outcomes of home HFNC in the pediatric population.
Design/Methods: A retrospective review of all children on home HFNC between 2013-2023 was conducted at a tertiary care pediatric hospital in Ontario, Canada. Descriptive statistics were used to summarize results. Wilcoxon signed-rank test compared acute care utilization in the year following and year prior home HFNC initiation.
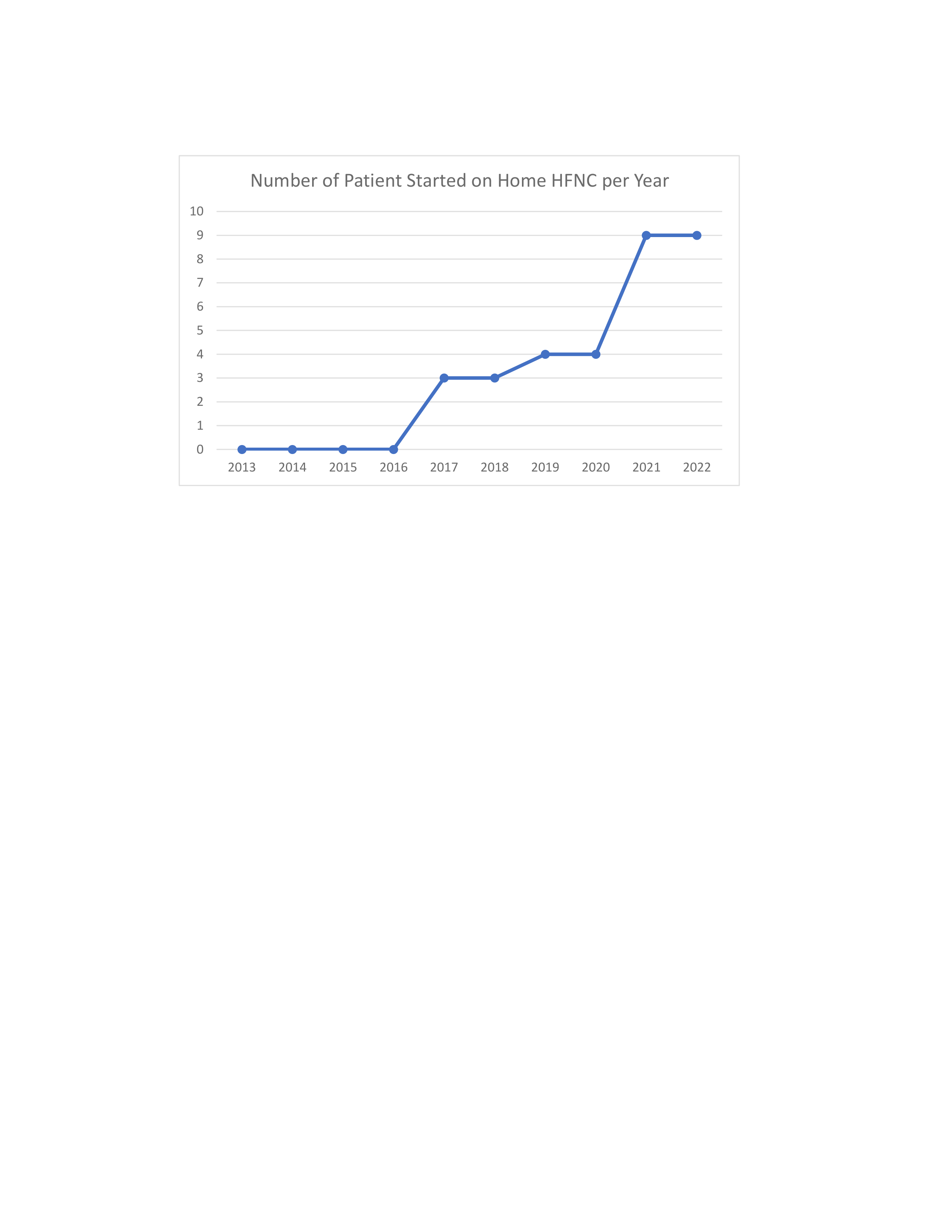
Results: A total of 35 patients, age 6 months–14 years old, were started on home HFNC between 2013-2023, with a gradual increase in use during that period (Figure 1). Home HFNC was almost exclusively prescribed in patients with multisystem conditions; n=27 (77%) with an underlying genetic disorder and 77% (n=27) with prior home feeding tube use.
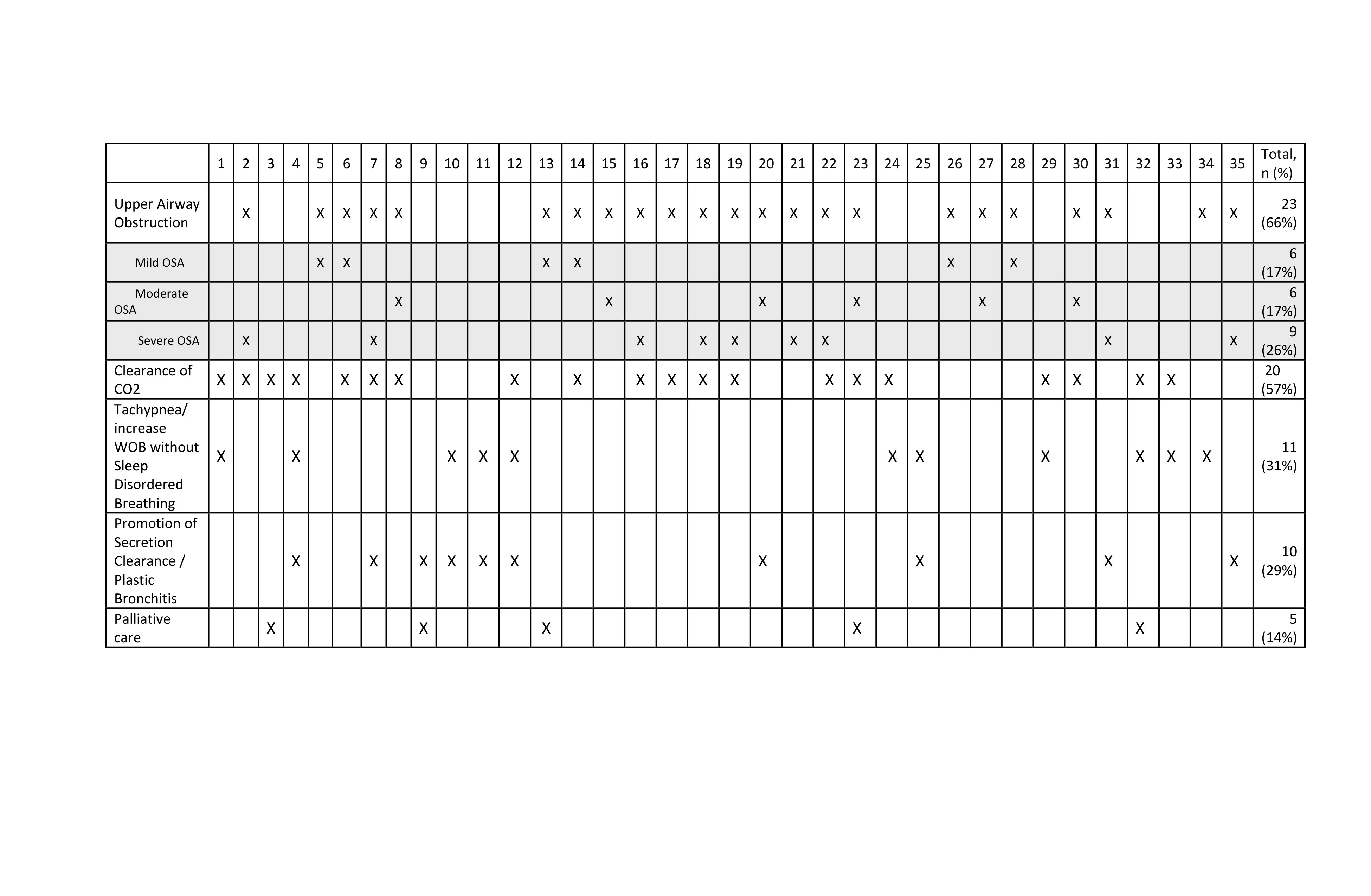
Table 1 outlines the indications for initiating home HFNC for each patient. The main indications to initiate home HFNC included: (i) upper airway obstruction (66%), (ii) clearance of CO2 (57%) (iii) increased work of breathing without sleep disordered breathing (31%), (iv) promotion of secretion clearance/plastic bronchitis (29%), and (v) palliative care (14%). In addition, 23% (n=8) did not tolerate previous trial of Continuous/ Bi-Level Positive Airway Pressure (CPAP/BiPAP). Most (83%, n=29) had multiple indications leading to the initiation of home HFNC.
An escalation in home respiratory supports to CPAP/BiPAP was required in 12% (n=4). Home HFNC was successfully discontinued for > 4weeks in 12% (n=4). Among those where HFNC was discontinued, the median duration of home HFNC use was 10.3 months (interquartile range 10.9). Only 2 patients (6%) experienced a home HFNC-related complications (epistaxis leading to an ED visit). Finally, there was no statistically significant difference in utilization of acute care services in the year following vs prior to home HFNC initiation (Table 2).
Conclusion(s): HFNC is increasingly being used among children and youth in the home setting, and generally for prolonged durations. Despite varied indications for home HFNC initiation, it appears to be safe, with few complications or need for escalation of therapy. Further research on clinical outcomes and impact on quality of life are required.
.png)