Medical Education
Session: Medical Education 7
440 - Increasing Pediatric Resident Satisfaction with Education in the Neonatal Intensive Care Unit
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 440
Publication Number: 440.1452
Publication Number: 440.1452

Morgan E. Hill, MD (she/her/hers)
Assistant Professor of Pediatrics, Division of Neonatology
Cincinnati Children's Hospital Medical Center
Loveland, Ohio, United States
Presenting Author(s)
Background: Pediatric residents are required to gain critical knowledge on fetal and neonatal care as specified by the American Board of Pediatrics (ABP). Yet with changing residency requirements, many complete training with only 8 weeks of Neonatal Intensive Care Unit (NICU) experience. It is crucial to maximize this limited educational experience. Utilizing fellows as teachers and promoting active learning are two ways to optimize education.
Objective: In this study, we aim to improve pediatric resident knowledge of key fetal and neonatal medicine topics through the development of a novel, case-based learning curriculum. We also aim to increase resident satisfaction with the educational curriculum offered during their level III NICU rotation.
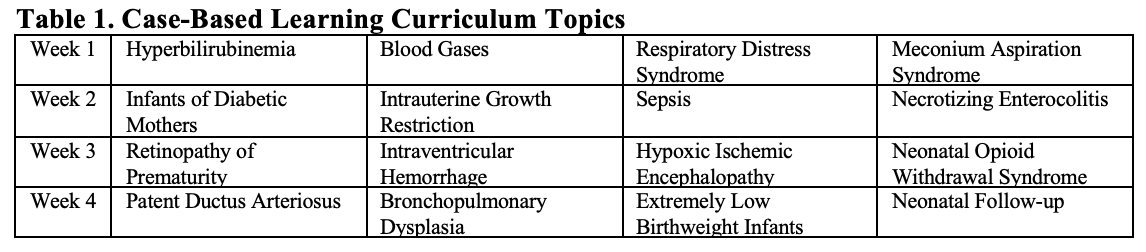
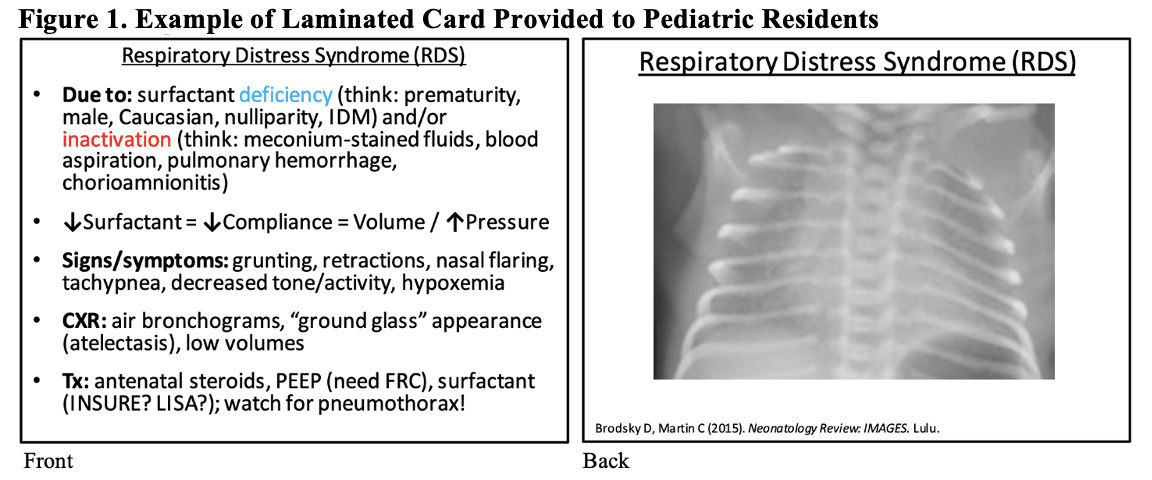
Design/Methods: A novel, case-based learning curriculum was developed that focuses on 16 key fetal and neonatal medicine topics (Table 1). These topics were chosen based on expert opinion of neonatologists, content covered in pediatric board-review questions, and as outlined by the ABP. Each topic was reviewed by the NICU service fellow as a case-based question immediately prior to morning rounds. Residents were then gifted a laminated card covering high yield learning points specific to the daily topic (Figure 1).
To assess effectiveness of and satisfaction with the curriculum, each resident completed a NICU Rotation Test and Education Evaluation Form on the last day of the rotation. Residents completed the test and evaluation before and after implementation of the novel curriculum. Summary statistics, Chi-square or Fisher’s exact test and non-parametric rank test were used as appropriate to describe the group differences.
Results: Eighty-three residents were evaluated, 47 pre-curriculum and 36 post-curriculum. No differences existed between the two groups in relation to prior NICU experience or residency training year. Test results did not improve after implementation of the novel curriculum, but education evaluation responses were significantly more positive (Table 2). Significantly more residents rated the overall teaching as excellent and strongly agreed that the appropriate topics were covered, the curriculum didn’t interfere with patient care, and the education facilitated learning. More residents believed the amount of time dedicated to teaching was just right.
Conclusion(s): A novel, case-based learning curriculum significantly improved pediatric resident satisfaction with the educational curriculum offered during their level III NICU rotation.
.png)
