Medical Education
Session: Medical Education 2
527 - Improvement in Neonatal Outcomes and Fellowship Satisfaction Scores after Adopting In-House Attending Coverage Model
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 527
Publication Number: 527.275
Publication Number: 527.275

Ravi Bhavsar, MD (he/him/his)
Neonatal Perinatal Medicine Fellow
University of Kentucky College of Medicine
Lexington, Kentucky, United States
Presenting Author(s)
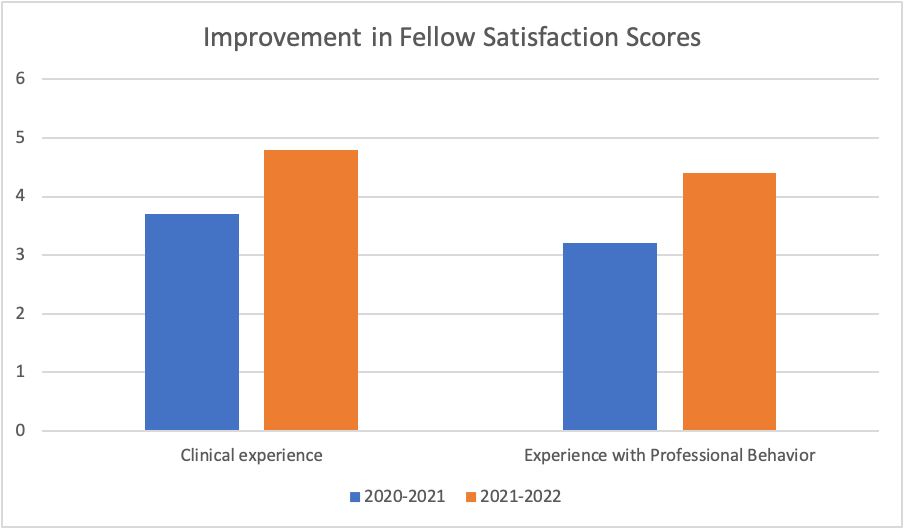
Background: Across the United States, more Level III and IV neonatal intensive care units (NICUs) are transitioning from attending at home night coverage to 24/7 in-house attending coverage. This has been largely due to an effort to improve both short and long-term neonatal outcomes, particularly in very low birth weight (VLBW) infants as well as the decreased time and experience pediatric residents now receive in the NICU. At our center, we transitioned to the in-house attending coverage model in 2021. There is no consensus among studies in NICU and Pediatric intensive care units that have adopted this approach, to indicate a clear improvement. There have also been concerns this approach may negatively impact fellow autonomy and learning. We hypothesized that in-house attending coverage would improve short-term outcomes and positively impact fellow education.
Objective: To compare short-term outcomes of newborns admitted to a tertiary Level IV NICU and to assess impact on fellow education following adoption of a 24/7 in-house coverage schedule.
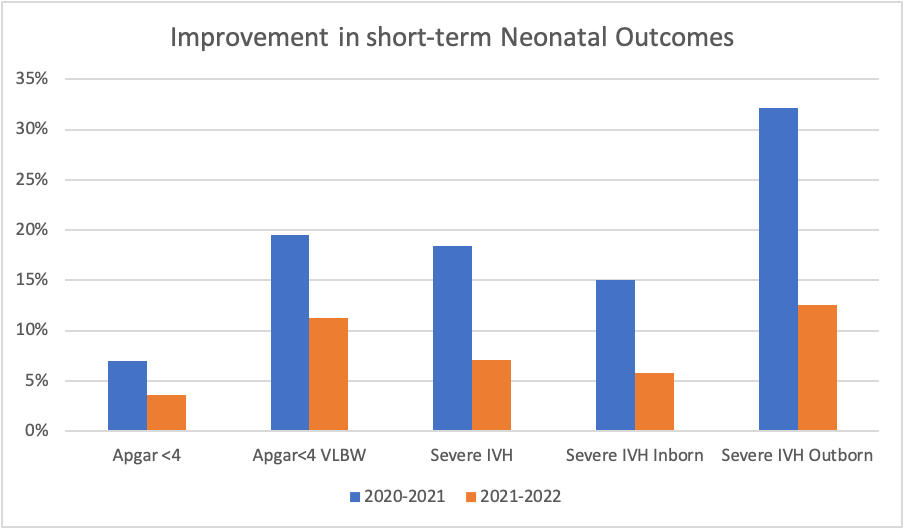
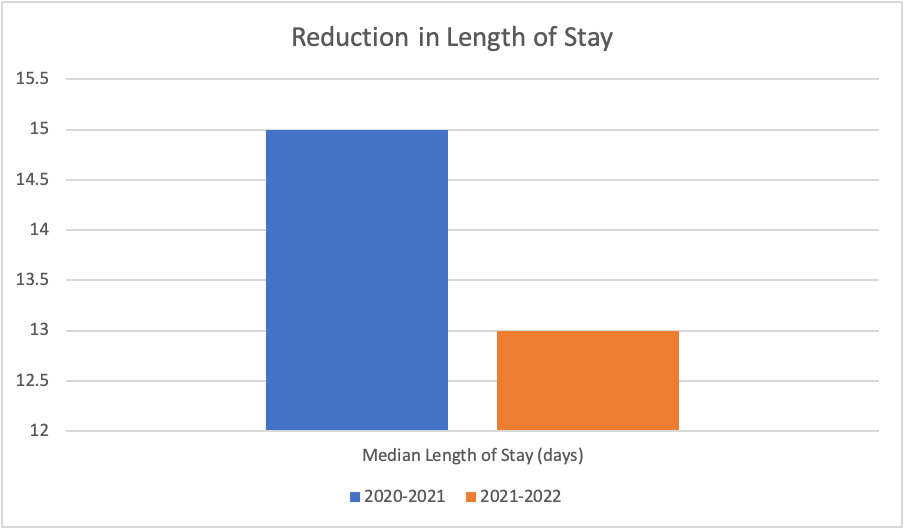
Design/Methods: An observational study comparing short-term clinical outcomes and impact on fellow education before and after implementation of in-house coverage mode in a 24-month period.We reviewed all neonates admitted to the University of Kentucky in the 24-month period from 2020-2022 and studied the differences in 5-minute Apgar scores. rates of severe Inter-ventricular Hemorrhage (IVH) and length of stay (LOS) in the NICU. We also compared the satisfaction scores of neonatal fellows based on clinical experience and modeling of professional behavior in both groups.
Results: The percentage of inborn infants who had an APGAR score of < 4 at 5 minutes of life decreased from 7%, prior to In-House Attending Call, to 3.6%. The percentage of VLBW inborn infants with a 5-minute APGAR score of < 4 decreased from 19.5% to 11.2%. The percentage of infants who had severe IVH decreased from 18.4% to 7.1%. (Inborn: 15% to 5.8%, Outborn: 32.1% to 12.5%). The overall LOS decreased from a median of 15 days to 13 days. Fellow satisfaction scores regarding their clinical experience improved from 3.7 out of 5 to 4.8 out of 5. Fellow satisfaction scores regarding their experience with professional behavior increased from 3.2 out of 5 to 4.8 out of 5.
Conclusion(s): Implementation of 24-hour in-hospital NICU attending coverage was associated with higher Apgar scores at 5 minutes of life, lower rates of severe IVH and an overall reduced length of stay. This also resulted in a positive impact on fellow education with improved satisfaction scores.