Neonatology
Session: Neonatal Follow-up 4
546 - Auditory Neuropathy Prevalence Rate and Post Discharge Hearing Outcomes in the NICU Population
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 546
Publication Number: 546.3109
Publication Number: 546.3109

Tiffany WS Lau, MD (she/her/hers)
Resident Physician
University of Hawaii, John A. Burns School of Medicine
University of Hawai'i at Manoa John A Burns School of Medicine
Honolulu, Hawaii, United States
Presenting Author(s)
Background: Auditory neuropathy (AN) is a type of sensorineural hearing loss (SNHL) that occurs when the inner ear detects sound but transmission does not occur to the auditory nerve. This is characterized by abnormal auditory brainstem responses (ABR) with normal otoacoustic emissions. NICU infants, particularly extremely preterm infants, have a high rate of auditory neuropathy, which is associated with hypoxia, hyperbilirubinemia, and other risk factors for sensorineural hearing loss. Management strategies in the NICU have changed, which may have impacted the rate of AN in these infants. The natural history of AN in this population is also unclear, with some evolving to SNHL and others completely normalizing.
Objective: To determine the current prevalence rate, evaluate risk factors, and determine the post discharge hearing outcomes of NICU infants with pre-discharge diagnosed AN.
Design/Methods: This retrospective case-controlled study examined infants admitted to Kapiolani Medical Center NICU from 2011 through 2020. Study infants were diagnosed with either AN or SNHL by diagnostic (dx) ABR prior to discharge. Control infants passed the newborn hearing screen and were matched to the study population by birth year, gestational age, and birth weight. Demographics and co-morbidities were compared for 38 AN, 86 SNHL and 248 control infants. Post discharge hearing outcomes were diagnosed by repeat diagnostic ABR 6 weeks after discharge.
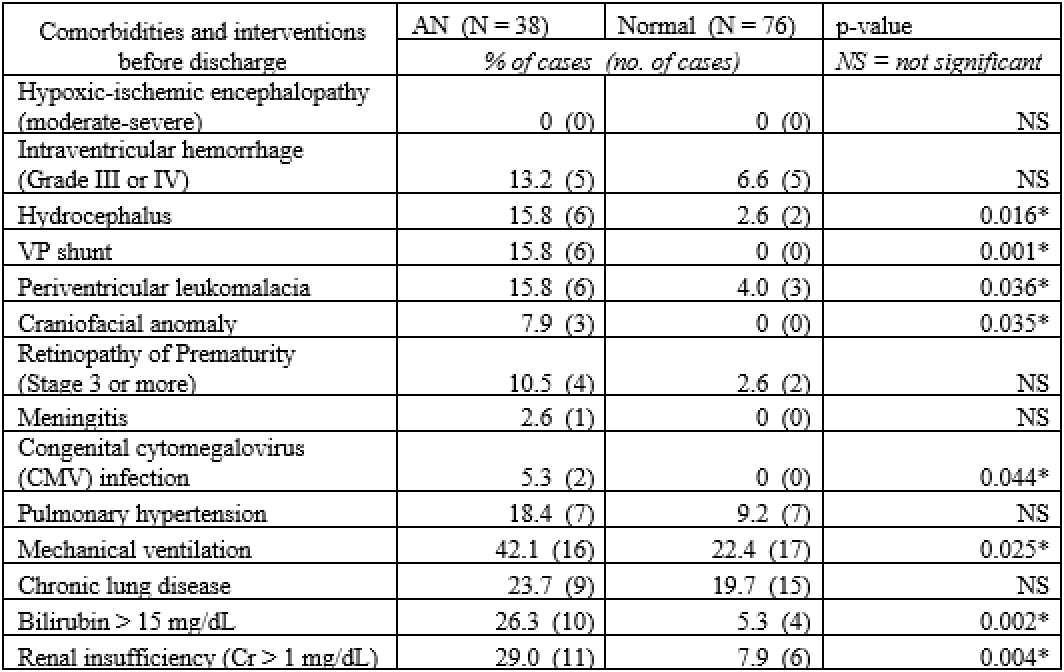
Results: In this NICU population, the overall prevalence rate of AN was 3.3/1000, while the rate of SNHL was 7.6/1000 infants. Extremely preterm infants had significantly higher rates of AN (16.3/1000) and SNHL (14.8/1000) vs older gestation infants (2.6/1000 and 7.3/1000 respectively) with p < 0.05 (Figure). Compared to age-matched controls, infants with AN had significantly higher rates of congenital CMV infection, craniofacial anomalies, renal insufficiency, and periventricular leukomalacia (p < 0.05). Significantly more AN infants required mechanical ventilation or had peak bilirubin levels > 15mg/dL (p < 0.05; Table).
When evaluated post discharge by repeat dx ABR, AN was confirmed in 23.7% of NICU infants with early diagnosed AN; 15.8% progressed to SNHL; while notably 42.1% were normal; and 18.4% were lost to follow up.
Conclusion(s): Consistent with previous reports, extremely preterm infants are at high risk for AN and SNHL. Higher severity of illness and major comorbidities are also significant risk factors. Early follow up is important as a significant number will show normal hearing on post discharge evaluation.
.png)