Newborn Care
Session: Newborn Care
217 - Evaluating the Impact of the Formula Shortage on Feeding Plans of Newborns
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 217
Publication Number: 217.280
Publication Number: 217.280

Jessica L. Knapp, MD (she/her/hers)
Resident
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: The formula shortage in 2022 came about from many different factors. The formula shortage had negative consequences including stress and the need for some families to change newborn feeding plans. It is not known if the formula shortage had a more lasting effect on a parent’s decision on how to feed their infant.
Objective: To determine if the recent formula shortage was a factor influencing the present feeding plans of newborns.
Design/Methods: A survey was created and validated by key stakeholders including neonatologists, general pediatricians, lactation consultants, and families. The survey was accessible on REDCap. Participants were a sample of convenience and consisted of delivered persons admitted to the post-partum unit or NICU at a single center starting July 2023. Exclusion criteria included any contraindication to breastfeeding, including positive HIV status and illicit substance use. Data from the survey were analyzed using Chi-squared categorical variables.
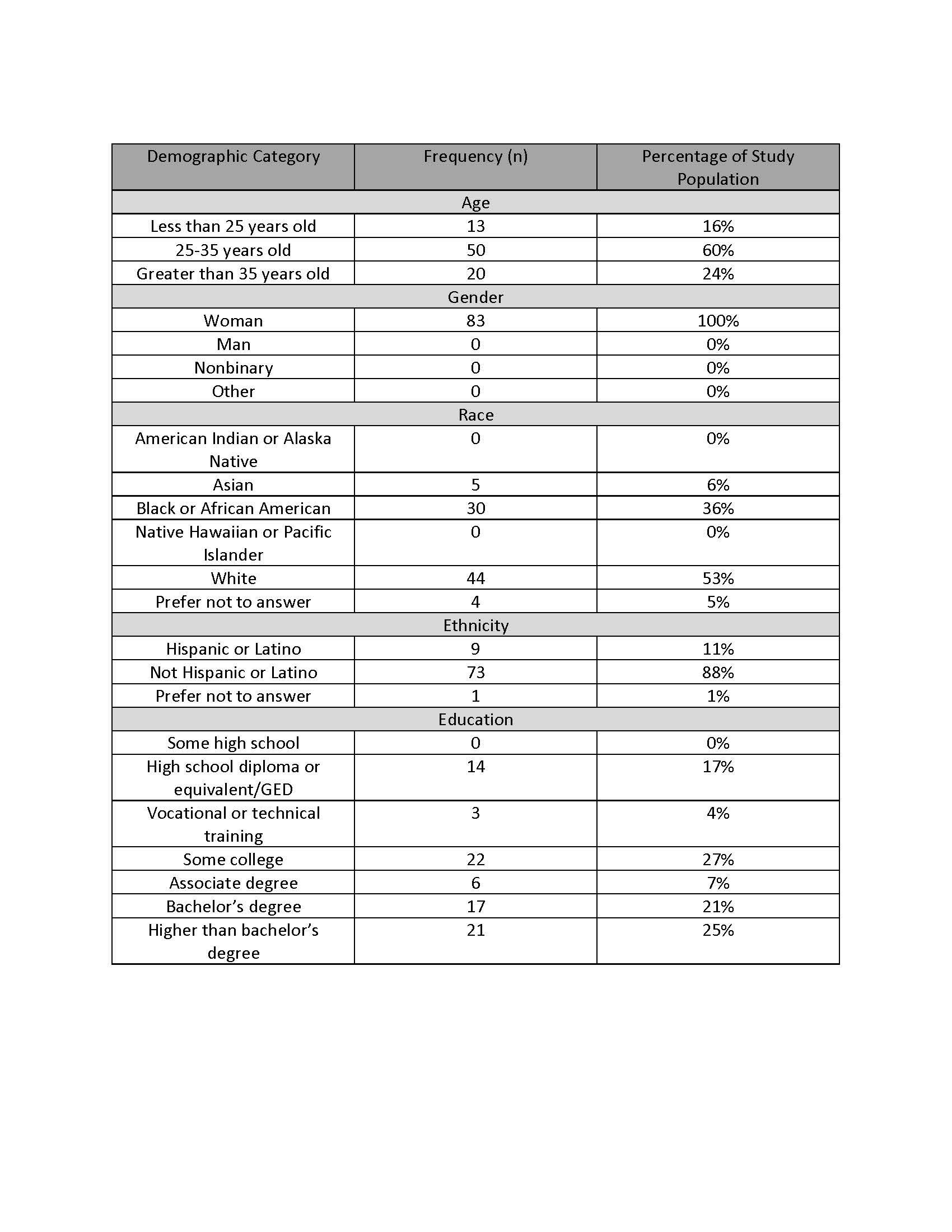
Results: The study sample included 83 participants (see Table 1). In the study sample, 49% of the surveyed population plan to exclusively breastfeed or offer breast milk to their baby, 45% plan to offer a combination of breast milk and formula, and 6% plan to use formula only. 86% (n=71) of participants were aware of the recent formula shortage, and 18% (n=15) agreed or strongly agreed that that the formula shortage impacted their decision to feed breastmilk or formula. Birthing persons >35 years of age (n=9, 45%, p=.03) were more likely to agree or strongly agree that that they were worried about the formula shortage making it hard to provide milk and indicated that there were other factors more important than the formula shortage in deciding how to feed (n=18, 90%, p<.01) compared to younger respondents. Those birthing persons with an advanced degree had a higher rate of agreeing or strongly agreeing that factors other than the formula shortage were more important in deciding how to feed (n-=19, 95%, P<.01) compared to those with less education. There were no differences in responses by race or ethnicity.
Conclusion(s): Our data show that while 86% of birthing persons are aware of the formula shortage, it influenced the feeding choices of 18% of study participants. While responses differed based on age and education, race and ethnicity did not influence survey responses. Our data are helpful to understand the ongoing ramifications of the formula shortage and help counsel families on infant feeding choices.