Child Abuse & Neglect
Session: Child Abuse & Neglect 1
175 - Osteogenesis imperfecta testing among young children presenting with long-bone fractures
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 175
Publication Number: 175.1435
Publication Number: 175.1435
- KF
Kristine Fortin, MD MPH
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Clinicians evaluating young children with long-bone fractures may question need for osteogenesis imperfecta (OI) testing as mild forms can present without apparent clinical features. There are currently no guidelines to help clinicians decide when to test for OI, which may result in variability and inequities in testing practices. We aim to better understand current OI testing practices.
Objective: Describe frequency and results of OI tests among children < 4 years with long bone fractures.
Compare demographic and clinical characteristics between children with and without OI tests.
Design/Methods: Sub-analysis of a multi-center prospective fracture model validation study of children with abusive and accidental fractures. We included patients at 3 pediatric emergency departments aged < 4 years with ≥1 long bone fracture. We excluded children injured by MVA and those with known OI. Completed laboratory test for OI (COL1A1/COL1A2, IFITM5) was the dependent variable. We defined abuse evaluation as completed child abuse pediatrician / social work consult, or skeletal survey. We conducted direct interviews, physical exams, and medical record reviews. We calculated frequency of OI tests and results. We used Chi-squared, Kruskal-Wallis, Fisher exact and t-tests to compare children with and without OI testing.
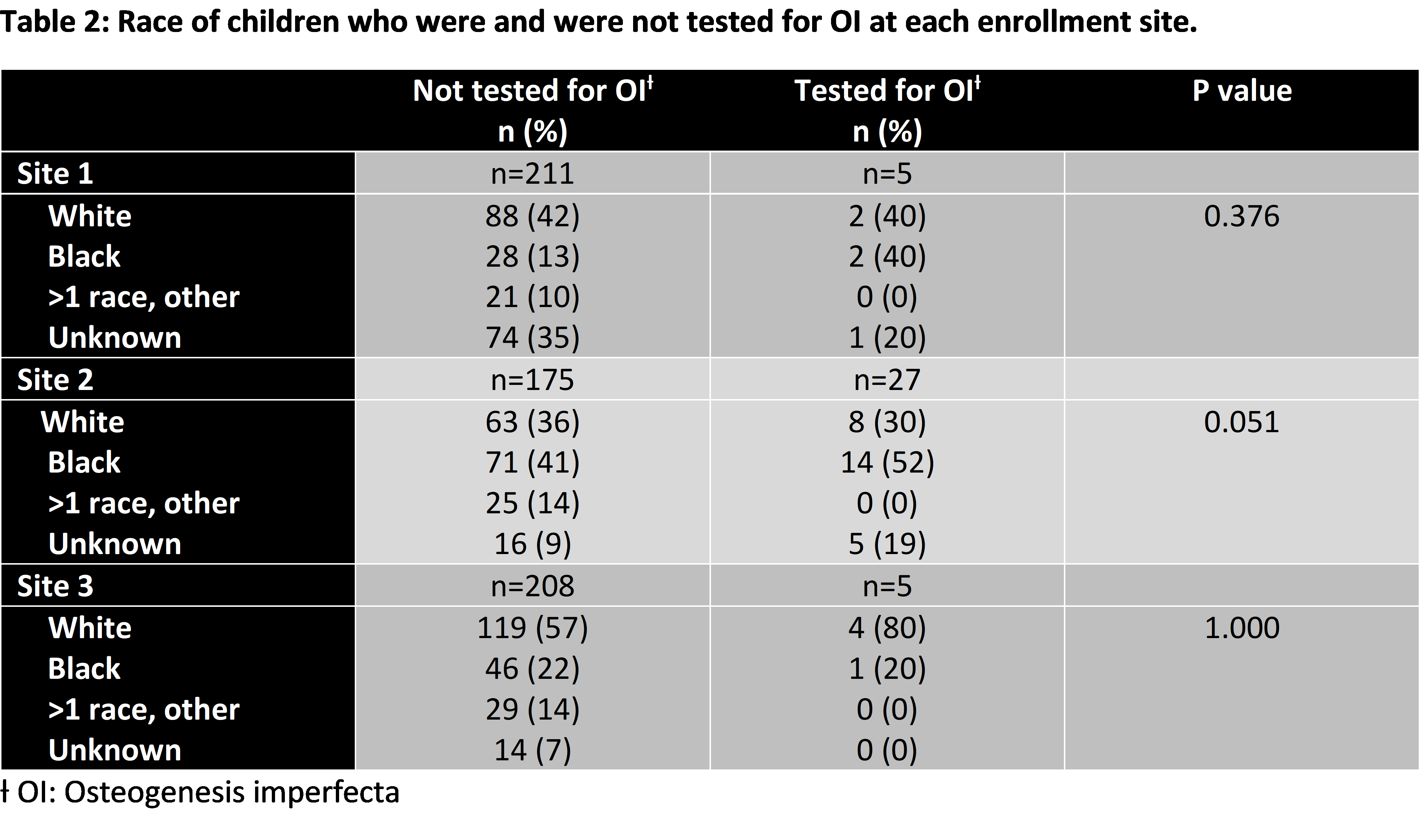
Results: In our sample of 631 children, 37 (6%) were tested for OI. Results were negative for 31 (84%), variant of unknown significance for 5 (13%) and positive for 1 patient (3%). Frequency of OI testing varied significantly across sites (Table 1). Almost all (97%) patients tested for OI were evaluated for abuse. Tested children were younger than those not tested, but insurance type did not differ significantly (Table 1). Race did not differ significantly by testing status within each site (Table 2).
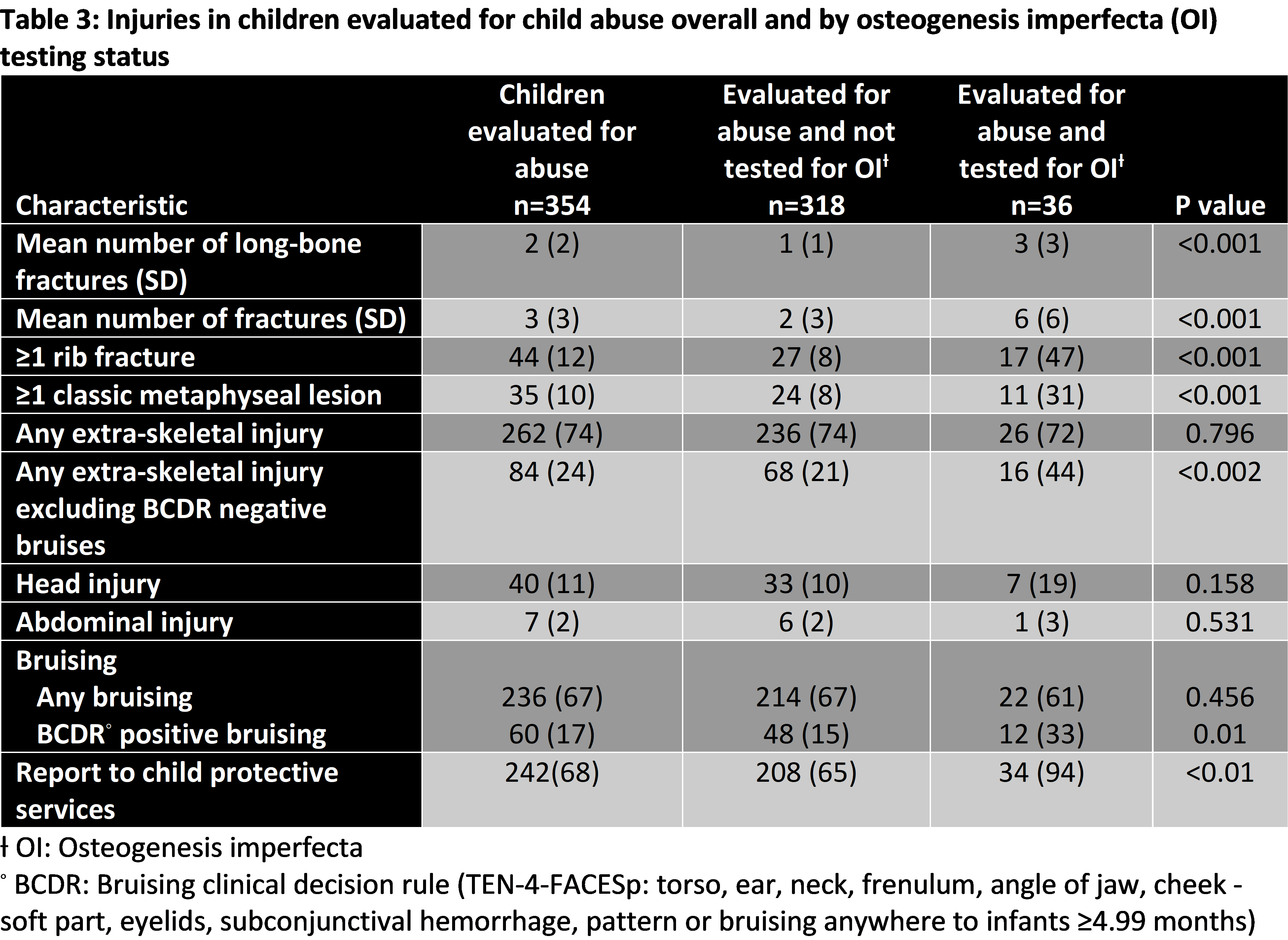
Table 3 details injuries sustained by children evaluated for abuse overall and by OI testing status. Children tested for OI had significantly more fractures compared to those not tested. Rib and classic metaphyseal lesions were more frequent in the former. Frequency of extra-skeletal injury did not differ significantly between the groups, except bruising with high specificity for abuse (positive TEN-4-FACESp bruising) occurred more frequently in tested children.
Conclusion(s): OI testing practices varied across sites. Testing was largely performed in the setting of abuse evaluations, including for children with injuries not typically associated with OI. Future directions include development of guidelines for OI testing, which could reduce practice variability and costs associated with low-yield testing.
.png)