Medical Education
Session: Medical Education 7
436 - Curation of a Resident-Centered Wellness Curriculum
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 436
Publication Number: 436.1426
Publication Number: 436.1426

Joseph B. Wall, MD (he/him/his)
Resident House Doctor
NewYork-Presbyterian Morgan Stanley Children's Hospital
NEW YORK, New York, United States
Presenting Author(s)
Background: Residents are at high risk for burnout, depression, and suicide. The ACGME recently required programs to address well-being - emphasizing psychological, emotional, and physical areas as being critical. It is unclear how successful programs are at identifying the needs of resident wellness and then addressing the root causes of those gaps. Certain specialties have created longitudinal curricula for resident wellness, but this is not standardized for pediatrics, which is a necessity.
Objective: (1) Perform a needs assessment to identify gaps. (2) Develop wellness curriculum and initiatives.
Design/Methods: Residents at a quaternary single institution completed a voluntary needs-assessment. Rank-scale and Likert questions were used to obtain information about which wellness topics are important, timing and frequency of didactics, and a wishlist for wellness initiatives. Survey data was evaluated using descriptive statistics. The results were used to create a resident focused wellness curriculum.
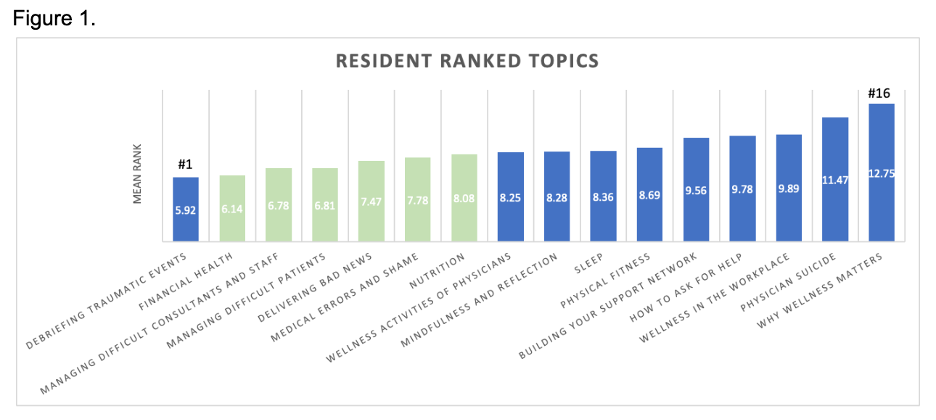
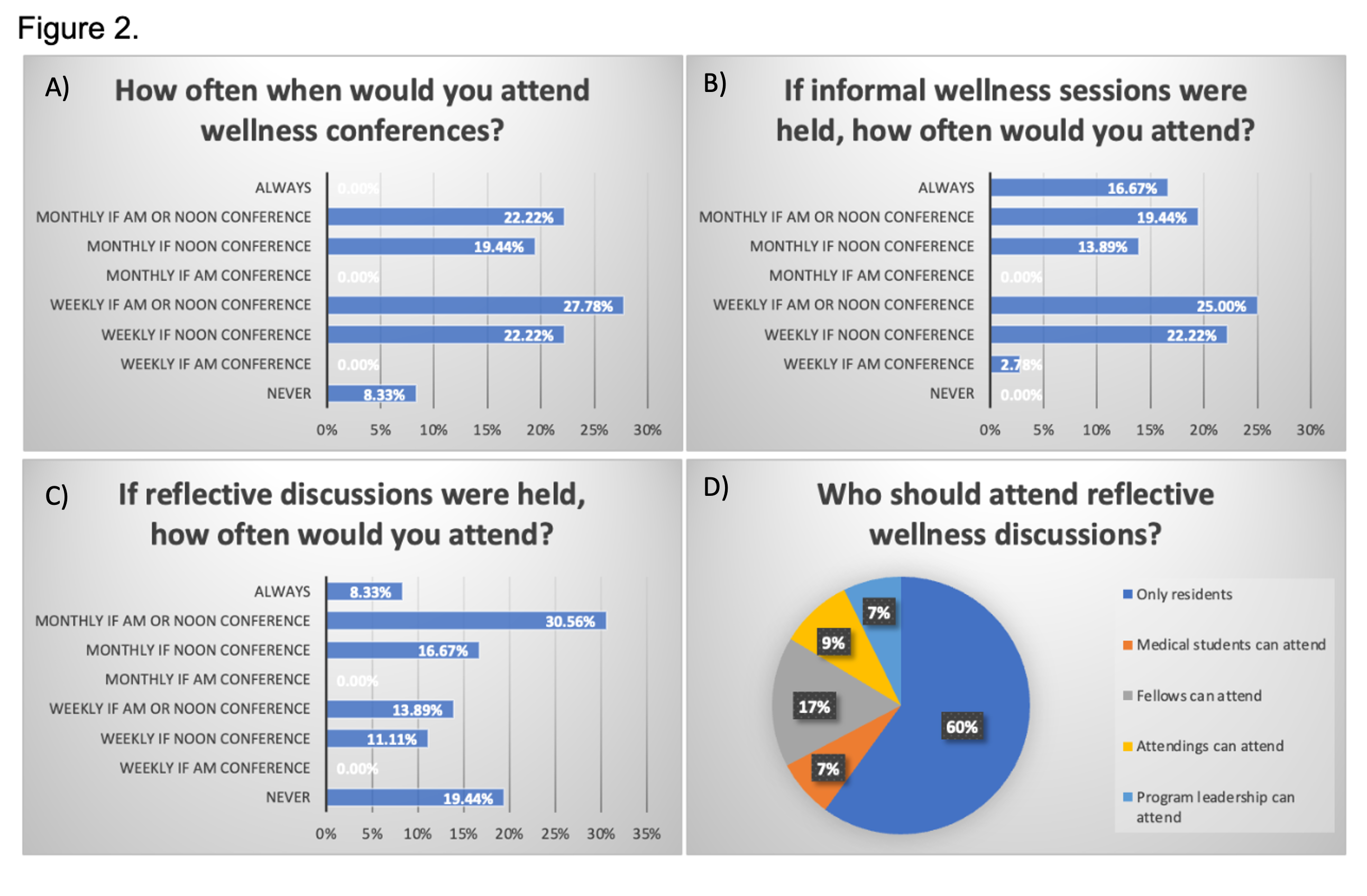
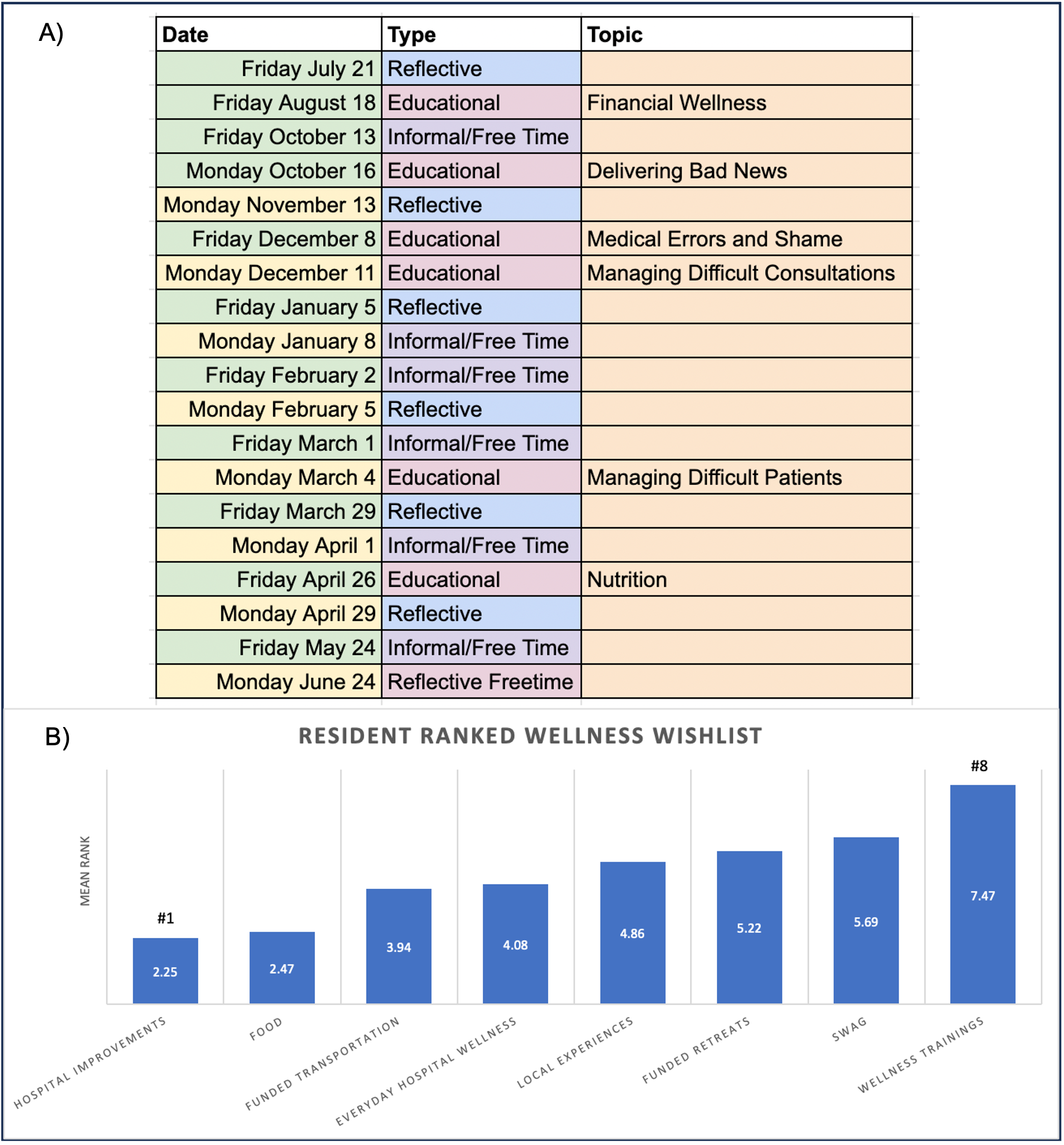
Results: The needs assessment response rate was 47% (N=36). Residents preferred conferences on practical skills for workplace challenges - debriefing traumatic events (rank 1, mean rank 5.92 + 4.5), financial health (6.14 + 3.3), and dealing with difficult situations (ranks 3-6) (Figure 1). Debriefing traumatic events was not included as it is implemented in other residency initiatives. Majority of residents were willing to participate in wellness conferences (Fig 2A), informal sessions for unstructured social time (2B), and reflective discussions to debrief in a safe space (2C). For reflective discussions residents preferred (60%) resident-only led sessions (2D). Based on the results, optional wellness sessions were held during pre-structured, protected conference time to not add to resident workload (Fig 3A). Practical needs such as hospital improvements, food, and transportation were selected as important funding requests (3B).
Conclusion(s): A resident-focused wellness curriculum was created based on a needs assessment. There was a preference for practical wellness skills rather than topics such as why wellness is important, mindfulness, and sleep. Of note, these were to be held during protected conference time. This is an important finding as previously perceived needs were different. Other programs would benefit from implementing a similar needs assessment. Future steps include evaluating the utility of the curriculum through surveys to further serve the needs of the residents. The resident wish list will be used for targeted grant proposals and funding opportunities to improve resident wellness.