Neonatology
Session: Neonatal Quality Improvement 3
416 - Golden Hour – Building Urgency to Provide Optimal Care for Neonates in a Level III NICU
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 416
Publication Number: 416.1931
Publication Number: 416.1931

Amie R. Ballard, MD (she/her/hers)
Neonatal Medical Director
Memorial Hermann the Woodlands
Spring, Texas, United States
Presenting Author(s)
Background: Children’s Memorial Hermann The Woodlands is a level III, 3600 delivery suburban Texas NICU with an average daily census of 25 babies. The “Golden Hour” concept in neonatology has shown that concerted initial resuscitative efforts in the first 60 minutes of life leads to improved short-term and long-term outcomes, especially in the tiniest babies. Despite awareness of the importance of Golden Hour care, we have found significant inconsistency in the initial care provided by our team, quantified by a wide range of time required to start intravenous fluids (IVF)/parenteral nutrition (PN) and high rates of initial hypoglycemia in qualifying infants.
Objective: To define Golden Hour patients as infants born at < 1500g or < 30 weeks
To design a multidisciplinary process to expedite NICU admissions for Golden Hour patients, with goals of IVF initiated within 60 minutes after birth and reduction of hypoglycemia to < 30%
To create a sense of urgency with very low birth weight (VLBW) admissions
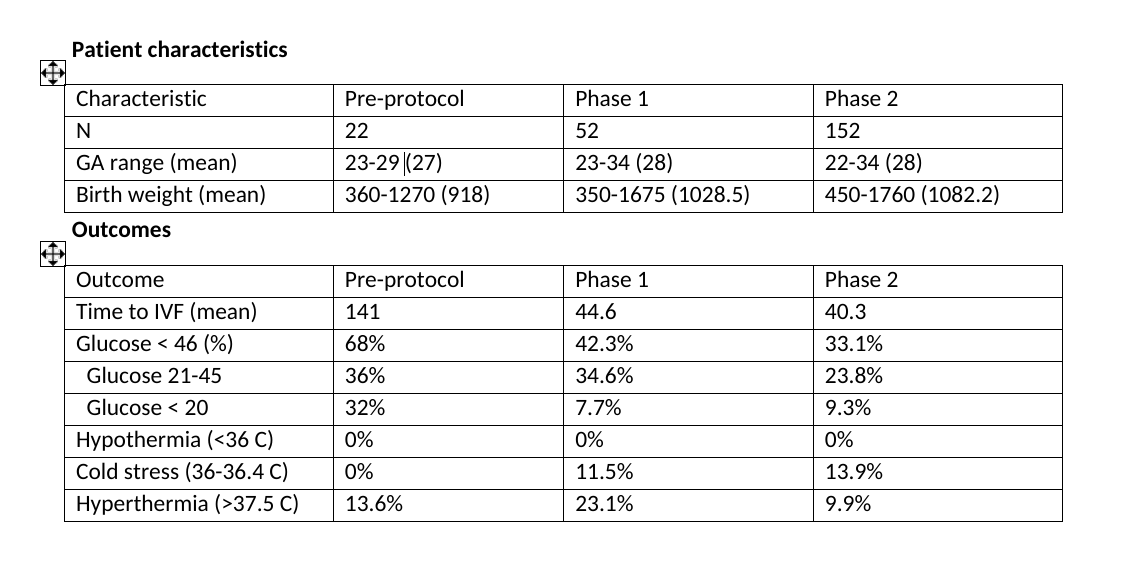
Design/Methods: A multidisciplinary team from nursing, clinicians, pharmacy, and NICU leadership met and defined specific roles for each member of the Golden Hour team. Tracking sheets for the NICU and pharmacy were developed. Using quality improvement methodology with multiple PDSA cycles, the Golden Hour protocol was implemented for all inborn infants < 30 weeks and/or < 1500g at birth. Data were collected (2019-2023) over three phases: pre-protocol (n = 22), Phase 1 with focus on time from birth to start of IVF/PN (n = 52), and Phase 2 with focus on time from birth to top down of the isolette, indicating completion of all Golden Hour tasks (n = 152). Admission temperature and percentage of babies hyperthermic or hypothermic were tracked as balancing measures.
Results: We observed significant improvements in minutes to start IVF/PN [mean 141 (pre-protocol) vs 44.3 (Phase 1) vs 40.3 (Phase 2)], and a reduction in hypoglycemia (68% vs 42.3% vs 33.1%). In Phase 2, time to top down of isolette decreased from 72.7 minutes (n = 29) in the first quarter to 59.6 minutes (n = 12) in the most recent quarter, mean 60.4 minutes (n = 152). Rates of hypothermia (11.5% vs 13.9%) were similar in both Phase 1 and Phase 2, but hyperthemia rates decreased (23.1% vs 9.9%).
Conclusion(s): Implementation of an evidence-based, multidisciplinary Golden Hour protocol is an effective way of reducing hypoglycemia and expediting IVF/PN initiation in preterm infants at a busy level-III community hospital. Adding the focus of time from birth to top down of the isolette further reduced time to start IVF/PN in these vulnerable infants.
.png)
.png)
