Hospital Medicine
Session: Hospital Medicine 1
307 - Feeding Intolerance in Children with Severe Neurological Impairment: The Development of a Clinical Practice Guideline
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 307
Publication Number: 307.312
Publication Number: 307.312

Justin Lam, MD, FRCPC, PhD Student (he/him/his)
Academic General Paediatrics Fellow
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Feeding intolerance (FI) in children with severe neurologic impairment (SNI) is a common problem in both inpatient and outpatient settings. Children with SNI often have serious feeding difficulties that can result in undernutrition, reduced quality of life, and increased healthcare use and caregiving needs. Despite the prevalence and importance of this issue, there is a lack of high-quality evidence and guidelines to improve patient and health systems outcomes.
Objective: The objective is to report on the development process of a clinical practice guideline (CPG) addressing FI in children with SNI.
Design/Methods: A multidisciplinary team with a background in complex care paediatrics, gastroenterology, hepatology & nutrition, dietetics, occupational therapy, pharmacy, nursing, interventional radiology, surgery, and palliative care, with expertise in caring for children with SNI, developed the CPG. First, a core, expert group took a collaborative, consensus-based approach to integrate evidence from existing observational studies, clinical practice guidelines, and local expert opinion. Additional experts then independently reviewed the CPG for clarity, accuracy, and to identify areas for improvement. To outline the strength of evidence and recommendations in our CPG, two authors independently reviewed and cited relevant recommendations in published CPGs. The intended end users were hospital-based clinicians and healthcare providers caring for children with SNI.
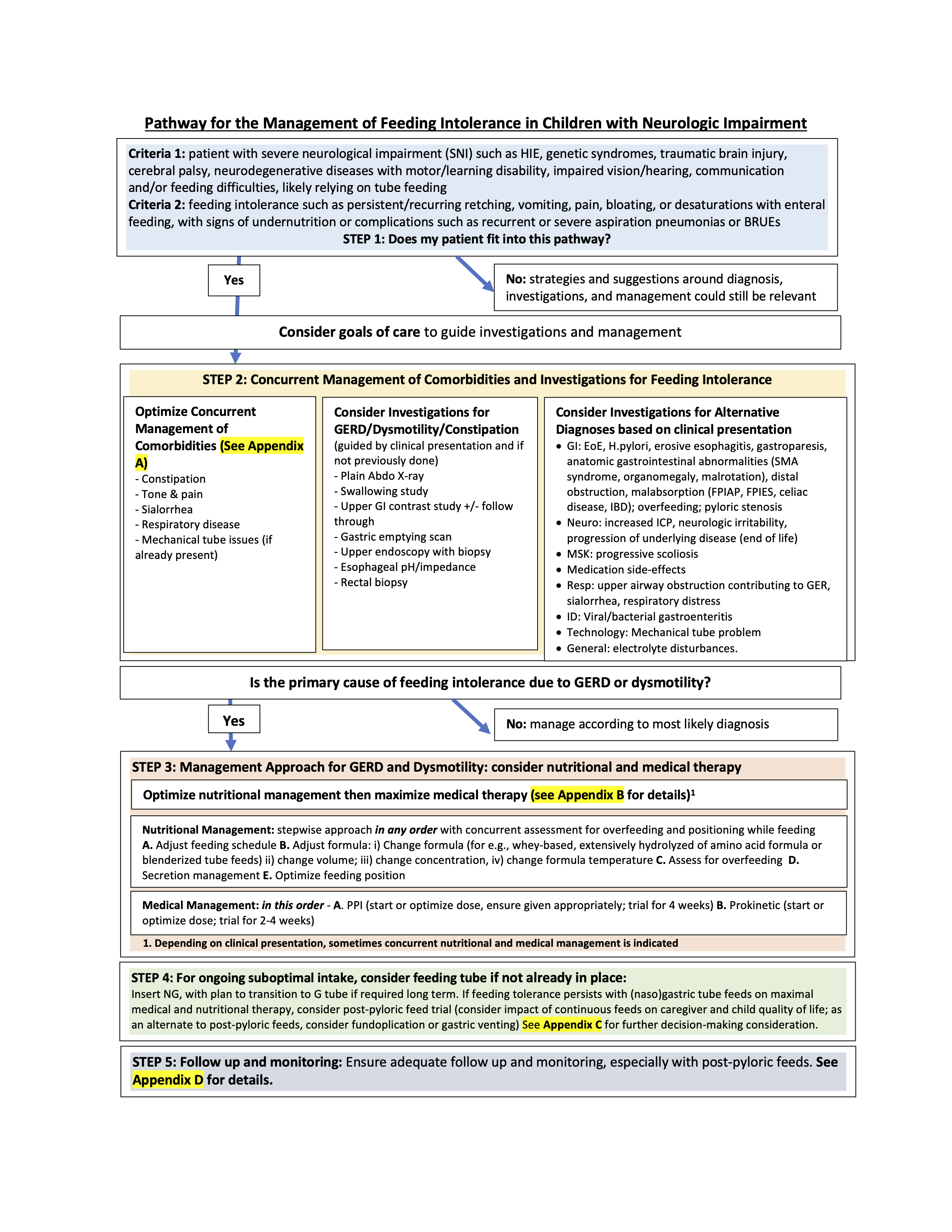
Results: The CPG outlines a suggested management approach for FI in children with SNI with 54 recommendations, and is summarized in a one-page algorithm (Figure 1). The CPG defines the population and FI, and discusses ethical considerations and patient goals of care. The CPG then reviews potential differential diagnoses for FI, identifies common comorbidities that affect FI, suggests strategies for concurrent management, and outlines the indications and limitations of diagnostic interventions for GERD and dysmotility as causes for FI. The CPG provides management approaches for GERD and dysmotility in children with SNI, including strategies for optimizing nutritional management and maximizing medical therapy. Finally, the document reviews feeding tube considerations. Thirty-one of 54 recommendations were accompanied by grading of evidence and recommendation strength.
Conclusion(s): A CPG was developed using a consensus-based approach in a multidisciplinary team of experts to address the management of feeding intolerance in children with SNI. Future work includes guideline implementation, evaluation, and dissemination.