Children with Chronic Conditions
Session: Children with Chronic Conditions 1
256 - Characteristics and Outcomes of Home Parenteral Nutrition among Children with Severe Neurological Impairment
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 256
Publication Number: 256.314
Publication Number: 256.314
- DD
David D'Arienzo, MDCM
Academic General Pediatrics Fellow
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Children with severe neurological impairment (SNI) often experience gastrointestinal issues, despite the absence of primary digestive disorders. In a subset of children with SNI and non-primary digestive disorders, enteral nutrition is not tolerated, and home parenteral nutrition (HPN) may be initiated. The clinical characteristics and outcomes of HPN in children with SNI and non-primary digestive disorders remains unclear.
Objective: To describe the characteristics, secular trends, and outcomes of HPN use among children with SNI and non-primary digestive disorders from 2010-2023; and compare their outcomes to children with primary digestive disorders on HPN.
Design/Methods: A retrospective review of all children with SNI and non-primary digestive disorders, in whom HPN was initiated between 2010-2023, at a tertiary care pediatric hospital. Clinical, demographic and HPN-associated outcomes were collected from chart review. Chi-square tests compared HPN outcomes between SNI - non-primary digestive disorders vs children with primary digestive disorders. Wilcoxon signed-rank test compared acute care services utilization in the year prior and year following HPN initiation.
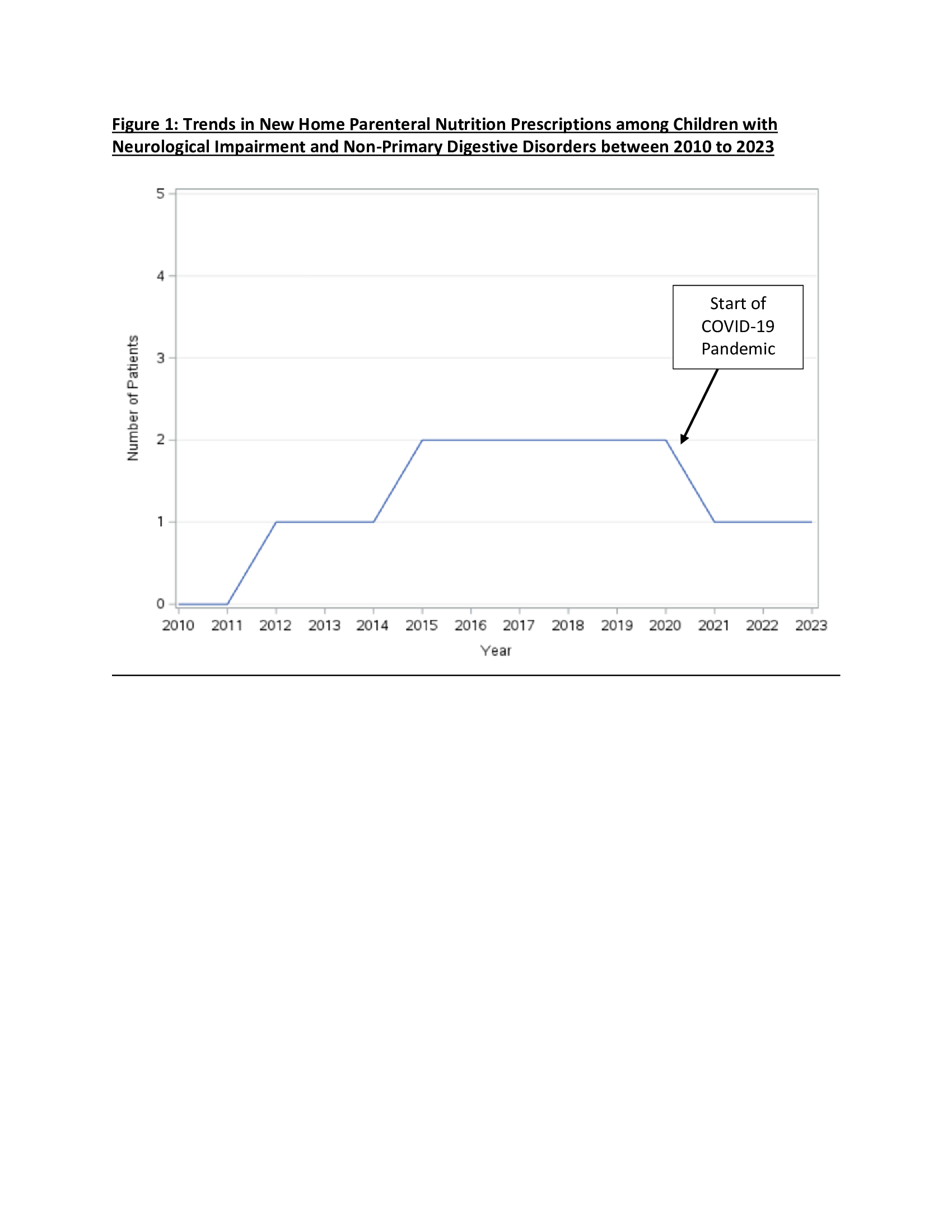
Results: Eighteen children with SNI and non-primary digestive disorders on HPN were included, with increasing use of HPN between 2010-2023 (Figure 1). The group was made up exclusively of patients with multisystem disease. Most patients (72%) had an underlying genetic condition and previous technology dependence (89% with prior home feeding tubes and 44% with prior home respiratory supports). Prolonged hospitalization was common at the time of HPN initiation [mean 104.2 (SD 64.9) days].
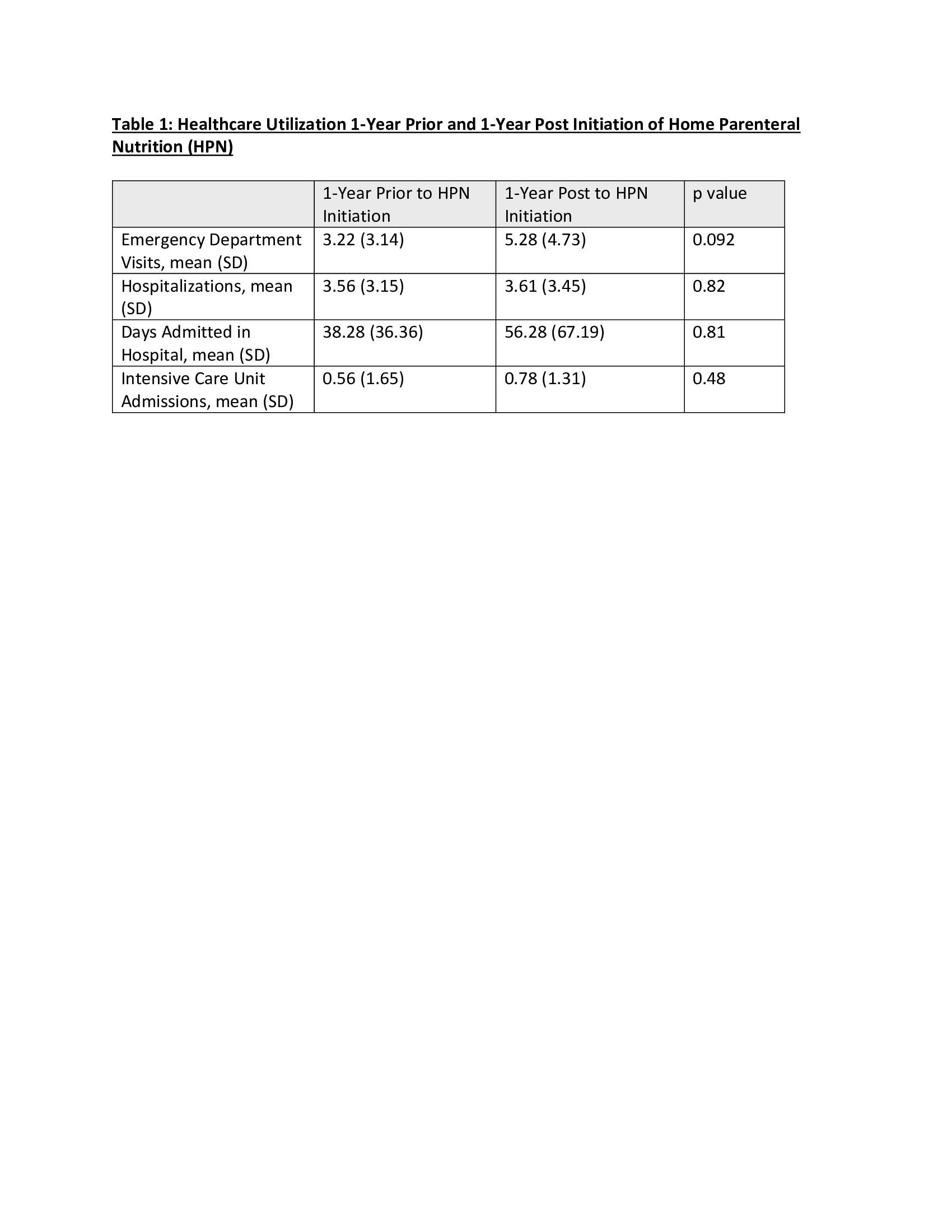
Among children with SNI and non-primary digestive disorder, 72% experienced a HPN-related complication (line-associated infection/thrombus, nephrolithiasis, cholelithiasis). Mortality occurred in 22%. Among those that achieved enteral autonomy (22%, n=4), the median duration on HPN was 12.9 months (interquartile range 39.6). Table 1 reports no statistically significant change in acute care utilization in the year prior vs year following HPN initiation. Compared with the primary digestive disorders group, children with SNI and non-primary digestive disorders were less likely to achieve enteral autonomy (p=0.001); however, mortality did not differ (p=0.31).
Conclusion(s): HPN is increasingly being used among SNI children with non-primary digestive disorders; however, complications are common. Compared with children with primary digestive disorders on HPN, children with SNI and non-primary digestive disorders are less like to achieve enteral autonomy.