Hospital Medicine
Session: Hospital Medicine 5
154 - Identifying Shifts in the Pediatric Hospital Medicine Job Market
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 154
Publication Number: 154.1394
Publication Number: 154.1394

Katherine Salada, MD (she/her/hers)
Assistant Professor
University of Michigan Mott Children's Hospital
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: Pediatric hospital medicine (PHM) was first approved as a sub-subspecialty in 2016 and an accredited fellowship in 2020. With this evolution, pediatric hospitalists can be board-certified/board-eligible (BC/BE) based on completion of a PHM fellowship or via the practice pathway (available only to those in practice by 2019). How PHM fellowship training and sub-specialty board eligibility affect career opportunities is currently unknown.
Objective: To describe potential differences in PHM hiring practices based on board eligibility or certification.
Design/Methods: An electronic survey was created with input from content experts at multiple institutions and administered to PHM leaders nationally via PHM listservs. The survey inquired about basic institution demographics, specific division characteristics, and hiring practices for the 2022-2023 recruitment season.
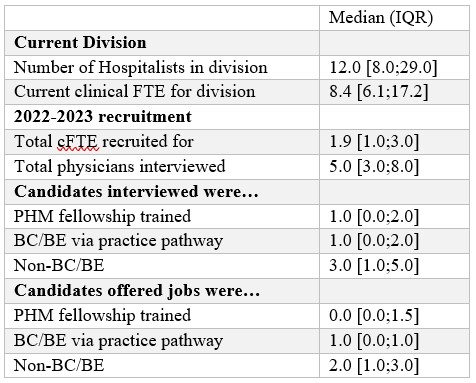
Results: 76 division leaders responded, representing a median division size of 12 hospitalists for 8.4 clinical FTE (cFTE). These divisions represent community (41%), university (37%), and combined (22%) sites (table 1). Most divisions (85%) reported over half of their currently employed hospitalists are BC/BE. PHM division directors interviewed a median of 5 (IQR 3-8) physicians to fill a median of 1.9 (IQR 1-3) available cFTE, with a variety of fellowship trained, practice pathway eligible, and non-BC/BE candidates (table 2).
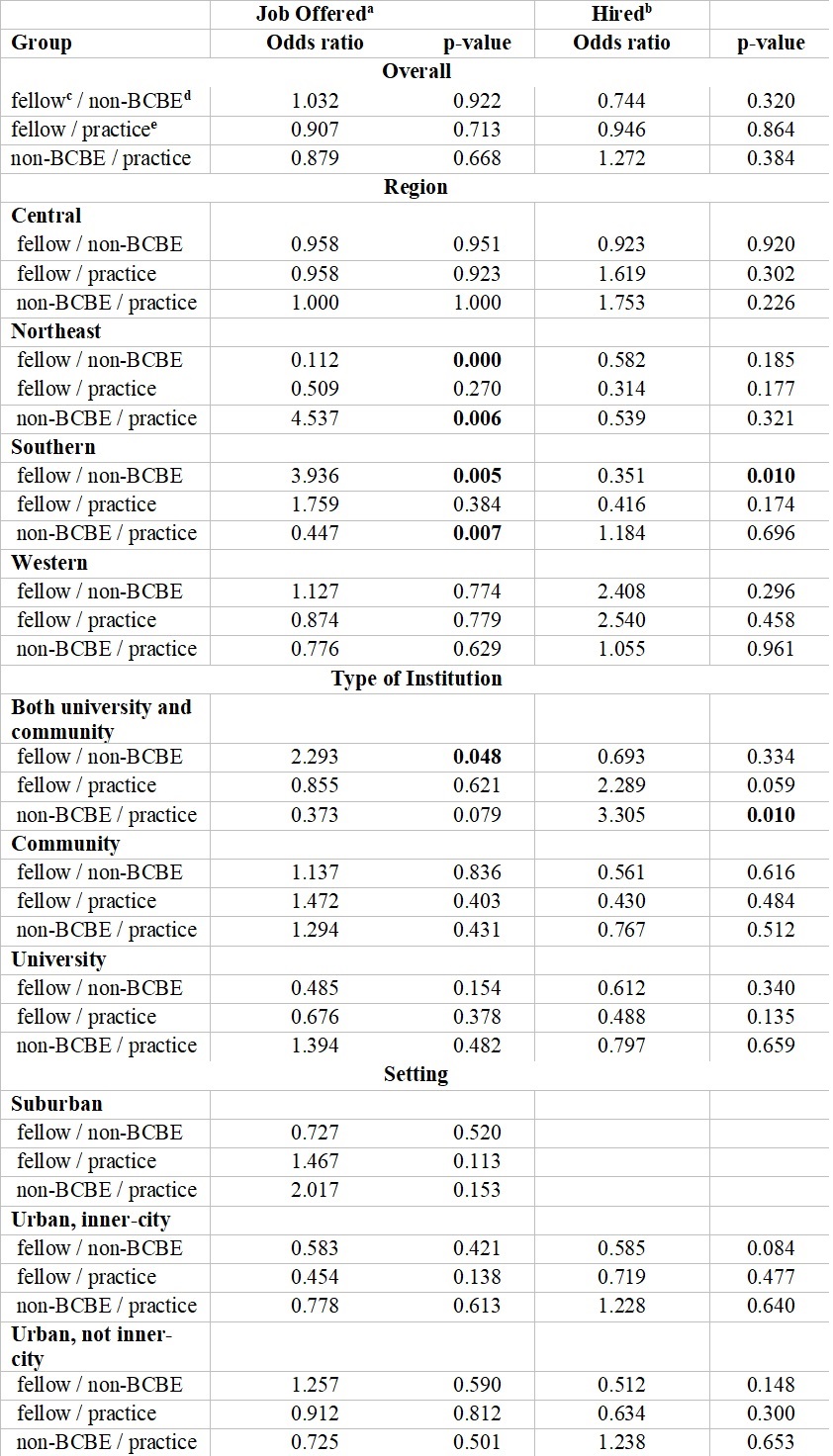
Overall, there was no difference in interviews extended, jobs offered, or candidates hired between fellow-trained, practice pathway eligible, and non-BC/BE candidates (Table 3). Non-BC/BE candidates were more likely to receive offers in the Northeast, but less likely to receive offers in the South, compared to either BC/BE group (fellowship-trained or practice pathway). Fellowship-trained candidates were more likely to receive offers at combined university/community sites than non-BC/BE (OR 2.30, p=.0.05), and non-BC/BE candidates were more likely to be hired than practice pathway candidates at combined university/community sites (OR 2.02, p=0.03). Hiring practices among BC/BE groups did not vary by hospital setting.
Conclusion(s): This study shows that non-BC/BE candidates continue to have a diverse array of job opportunities in PHM across the country. However, variability in PHM hiring practices by geographical region and type of institution have emerged among candidates from different BC/BE pathways. Further study is required to understand how these shifting trends in hiring impact learner training, faculty compensation, and academic productivity of PHM divisions.
.jpg)