Hospital Medicine
Session: Hospital Medicine 3
336 - Exploring Mechanisms That Drive Hospitalized Pediatric Patients and Families to Leave Against Medical Advice: A Qualitative Study
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 336
Publication Number: 336.328
Publication Number: 336.328
Rita Y. Wang, MD (she/her/hers)
Resident Physician
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Children leaving against medical advice (AMA) from the hospital pose challenging medical and ethical dilemmas for caregivers, families, and healthcare providers. Leaving AMA has been associated with adverse medical outcomes and readmissions. Limited research has explored underlying drivers leading to these risky discharges for pediatric patients in the US.
Objective: (1) To describe the characteristics of pediatric patients who left AMA from an urban safety-net hospital.
(2) To qualitatively assess contextual and mediating factors with care delivery surrounding leaving AMA.
Design/Methods: We performed a retrospective cohort study of patients < 18 years old and/or admitted to a pediatric service who left AMA from an urban safety-net hospital (1/1/2017-12/31/2022). Using summary statistics, we explored self-reported sociodemographics. We conducted qualitative content analyses of medical documentation to examine care provision and drivers underlying patients leaving AMA. Qualitative analyses included coding, theming, and summarizing stages. We identified representative stories to illustrate key themes through the patient and family voice.
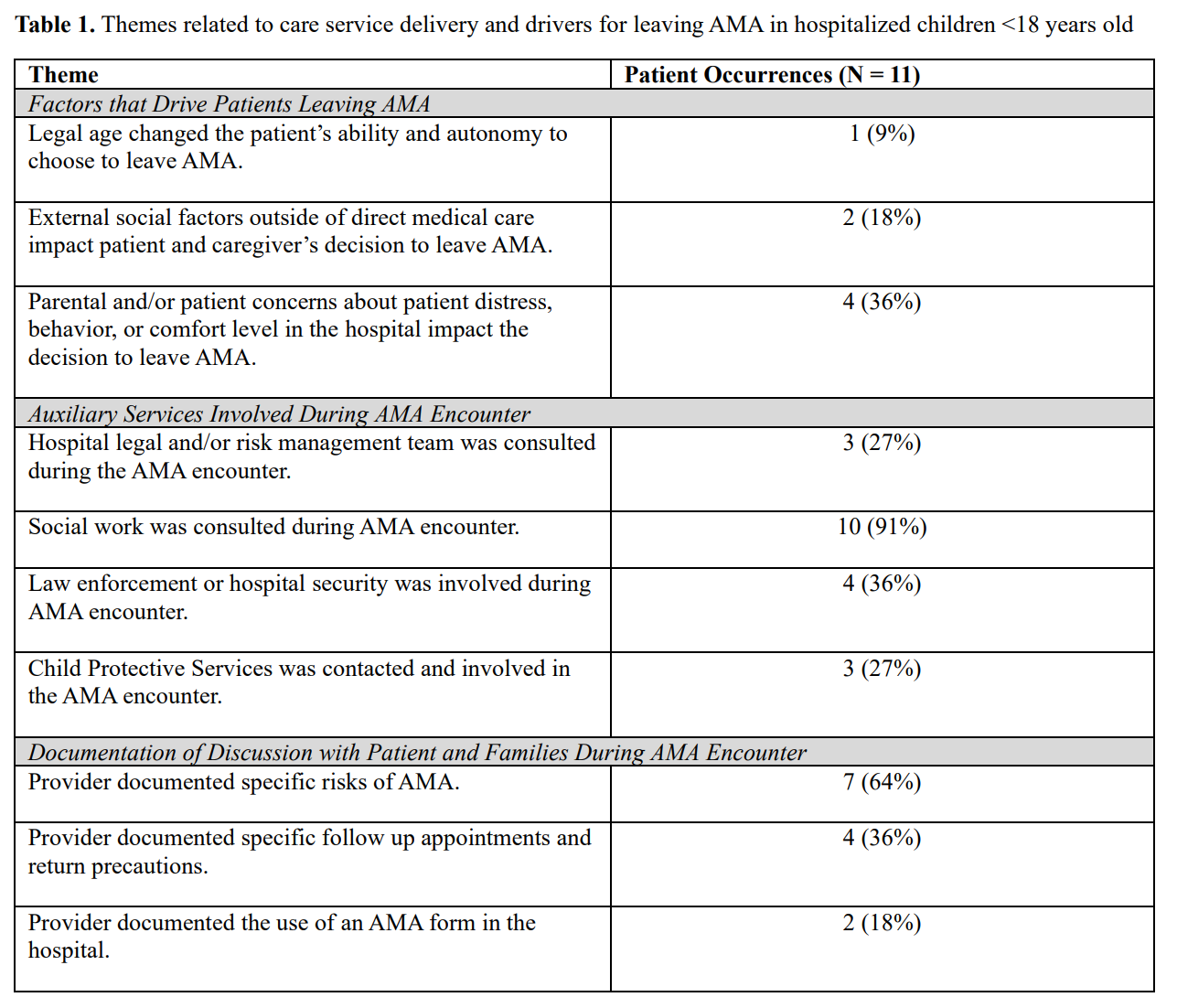
Results: Eleven patients < 18 years old left AMA during the studied time period. Most were ages 15-17 years (n=8, 73%), identified as Black (n=5, 45%) or Hispanic (n=3, 27%), had chief concern of mental health (n=3, 27%) or trauma (n=5, 45%), and had public insurance (n=11, 100%). Table 1 highlights key emerging themes from our content analysis relating to the driving factors for leaving AMA, auxiliary services involved, and documented provider-family conversation around leaving AMA. Identified drivers included legal age, external social stressors, and patient perception of hospitalization. Hospital encounters resulting in leaving AMA involved social work, child protective services, hospital security, and legal/risk management. While most discharge documentation summarized a discussion of specific health risks for patients leaving AMA, less than half discussed return precautions or steps taken to mitigate risky discharge. 64% of patients leaving AMA re-presented for care to the ED, inpatient readmission, or outpatient follow up within 14 days.
Conclusion(s): Although relatively uncommon, we found a high degree of medical, social, and ethical complexity that medical providers, caregivers, and patients grappled with during pediatric hospitalizations ending in leaving AMA. Heterogeneity in counseling and care services utilized during these hospitalizations highlights opportunities for health system improvements and standardization for these challenging discharges.