Hospital Medicine
Session: Hospital Medicine 4
133 - Capturing Complexity: Improving Length of Stay Index (LOSI) for Children Admitted with Respiratory Illness
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 133
Publication Number: 133.1390
Publication Number: 133.1390

M. Alex Ahearn, MD, MPH (he/him/his)
Clinical Assistant Professor
University of North Carolina at Chapel Hill School of Medicine
Chapel Hill, North Carolina, United States
Presenting Author(s)
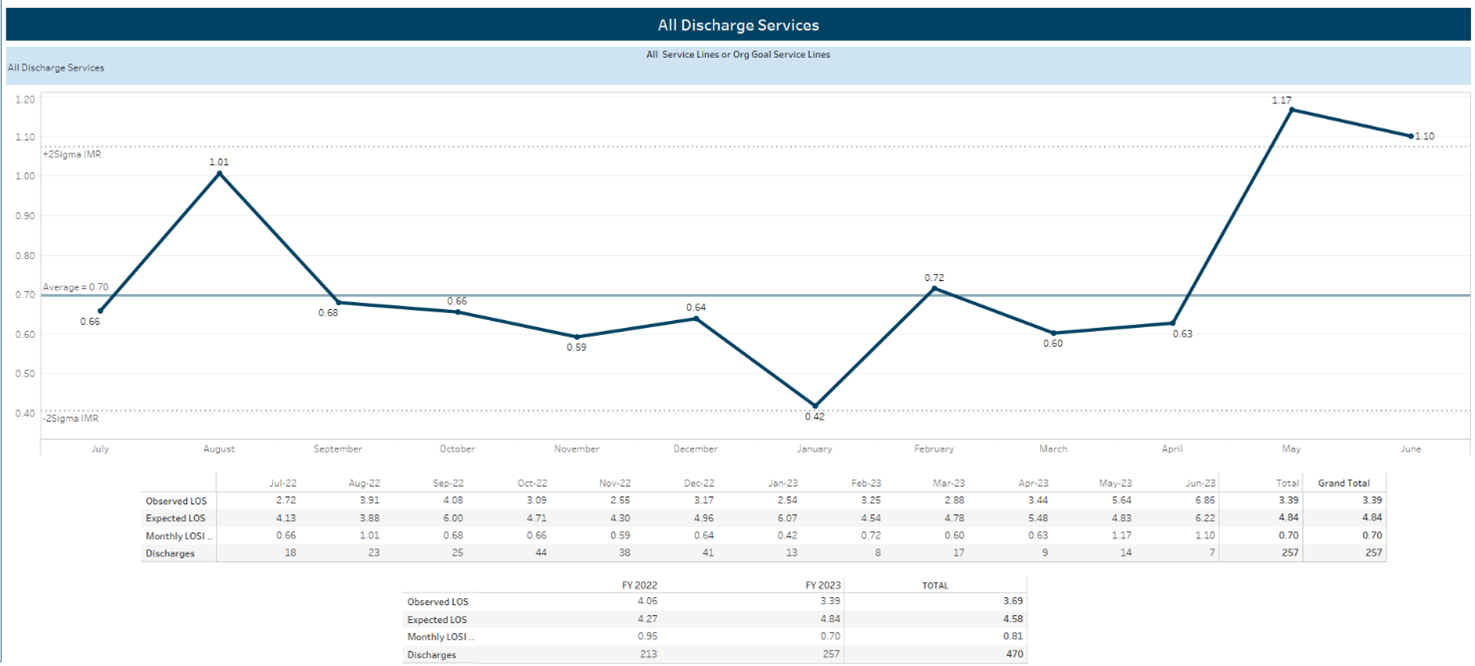
Background: Hospitals strive to provide high-quality care while responding to financial constraints. In our area, several pediatric units have closed and those remaining report bed and staffing shortages. Increased use of intensive respiratory support (e.g. high flow nasal cannula, HFNC) in non-intensive care settings has contributed to this strain. Length of stay index (LOSI, actual/expected LOS) at our institution was high during fiscal year 2022 (FY22 LOSI: 1.28) prompting an effort to reduce LOSI and maximize bed utilization. We focused our efforts on a high-volume population: patients with respiratory illness.
Objective: The aim was to decrease LOSI by 7% in FY23 for all patients on our acute care medical unit by focusing on children with respiratory illness.
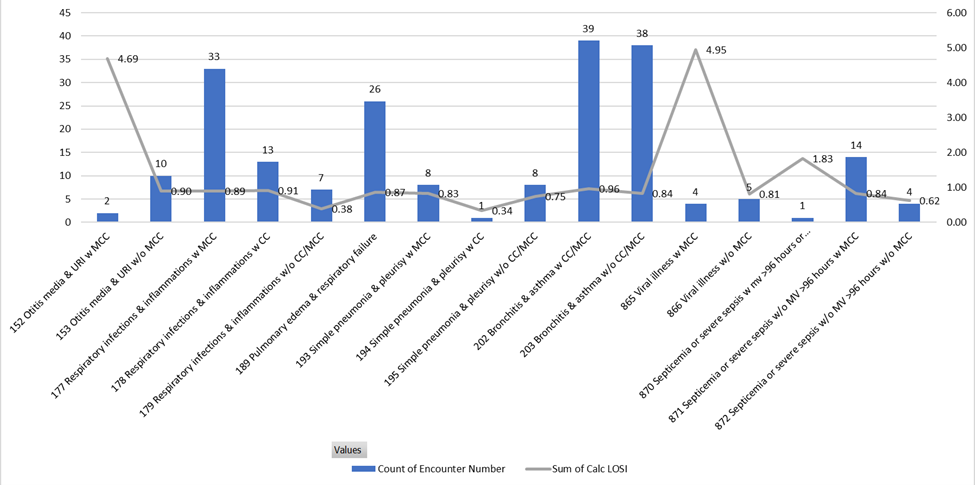
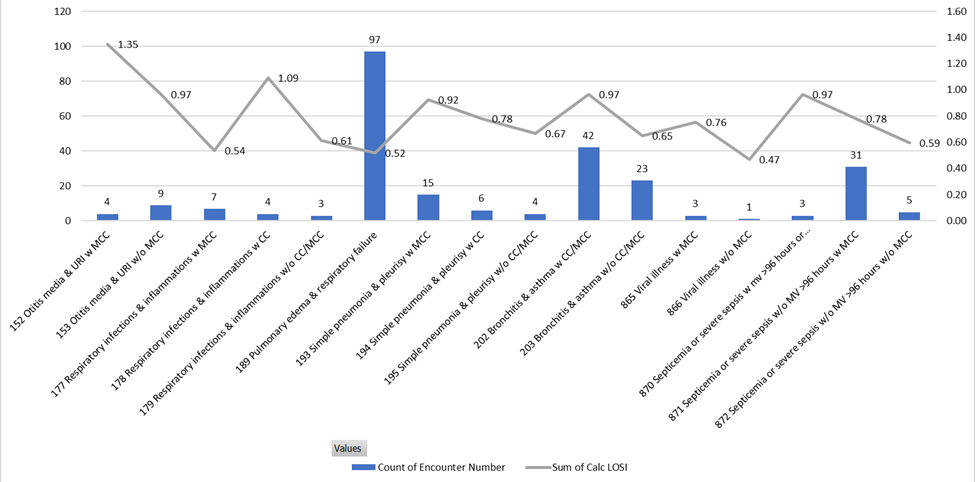
Design/Methods: Our multidisciplinary team used PDSA cycles to decrease LOSI. A clinical pathway (CP) with respiratory weaning guidelines existed at our institution, but adherence was poor. Interventions included: 1) additional training on the CP for all care team members, 2) integration of standardized respiratory assessments into patient flowsheets, 3) automated display of respiratory support to providers’ lists to identify discharge readiness, and 4) reeducation of providers by clinical documentation specialists to accurately capture patient complexity and disease severity.
Results: Patients with respiratory illness had a LOSI reduction of 26% (FY22: 0.95, FY23 target: 0.88; FY23 actual: 0.70) despite a 20% increase in admissions (FY22: 213; FY23: 257). Weaning of HFNC per CP guidelines nearly doubled across the observation period but remained low (baseline 6.5% -> 12.8%). Compliance with the CP for weaning LFNC was low and did not change significantly (baseline: 31% -> 30%). Time from patients meeting discharge criteria to placement of discharge orders decreased but did not reach goal (baseline 4:49 -> 4:16 hrs; target 4:00 hrs). Documentation and coding changes decreased the variance in diagnosis-related groups (DRGs) used for respiratory illness and increased the use of DRGs associated with more severe illness.
Conclusion(s): Over one year, LOSI decreased by 26% for acute care pediatric patients with respiratory illness and contributed to an overall 9% LOSI reduction for our acute care pediatric medical unit. Structured wean of respiratory support and improved communication yielded small improvements in factors that impact actual LOS (e.g. time to discharge orders, HFNC weaning), while other practices were unchanged (e.g. LFNC weaning). A notable factor in LOSI improvements was documentation and coding that more accurately identified severe illness.