Technology
Session: Technology 2
183 - Assessing Clinician Burnout and Electronic Health Record Usability Amongst Clinicians During Implementation of a New Electronic Health Record
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 183
Publication Number: 183.1960
Publication Number: 183.1960
- MS
Manan Shah, MD
Instructor
Robert Wood Johnson Medical School, Rutgers University
New Brunswick, New Jersey, United States
Presenting Author(s)
Background: Clinicians spend a large percentage of their time using Electronic Health Records (EHR), which has been shown to add to their stress and burnout. While the transition to a new EHR system may affect every aspect of the workflow, little is known about its effect on existing clinician burnout and perception of their job.
Objective: To examine the effects of a new EHR implementation on physician burnout over time.
Design/Methods: This study was conducted in an academic Children’s hospital, which underwent a transition from one EHR to another in June 2022. A survey was sent to physicians and nurses working in inpatient units at three time points: Period 1, before implementation; Period 2, two weeks after implementation; and Period 3, six months after implementation of the HER. Information was collected on baseline characteristics and validated Mini Z Burnout inventory to assess clinician burnout, and the system usability scale (SUS) to measure the usability of the EHRs was compared between three periods. We also collected qualitative responses on clinician perspectives of the implementation
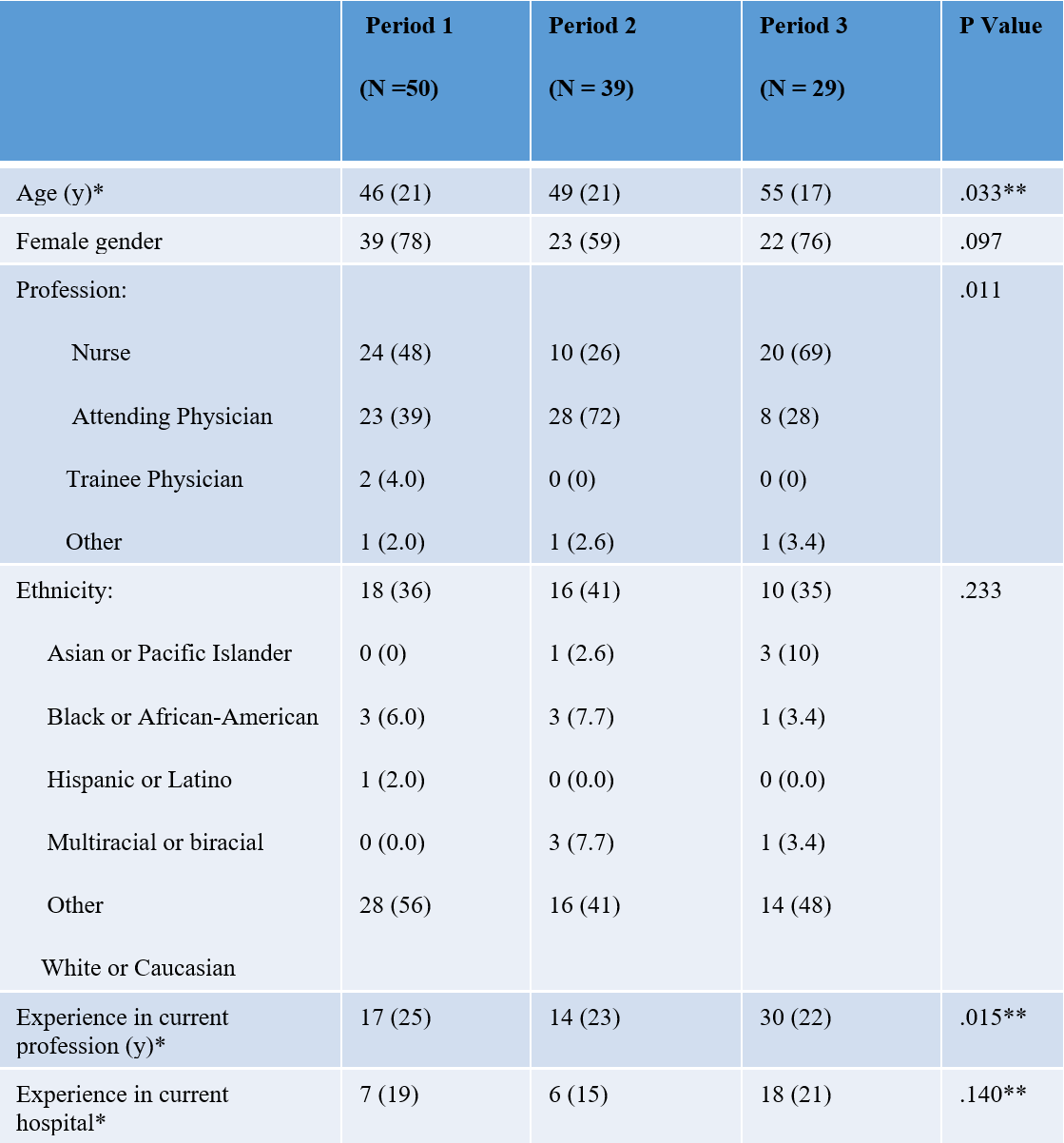
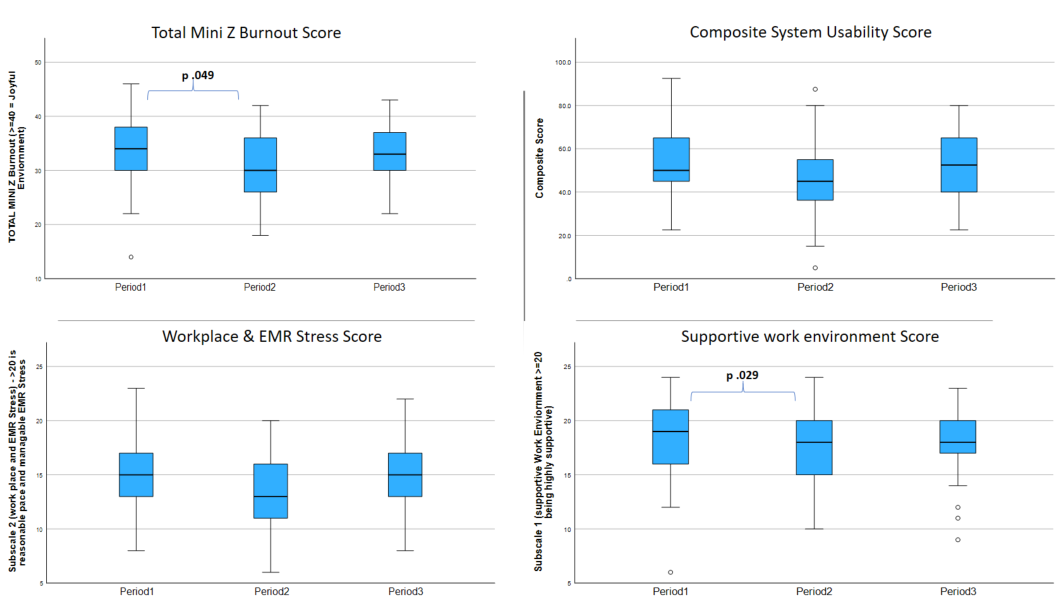
Results: There were 119 responses, with 51 during Period 1, 39 during Period 2, and 29 during Period 3, with significant differences in the median age and experience between the three periods. (Table 1) The ease of use of EHR and the number of clinicians reporting no symptoms of burnout was low throughout the three periods. A large majority of respondents disagreed that EHRs improve patient care, particularly those over 50 years of age (Table 2). There was an increase in burnout (p=0.049), as well as a perceived decrease in supportive work environment (p=0.029) during Period 2 as compared to Period 1. (Figure 1)
Qualitatively, some of the comments regarding EHR included “takes away time needed to care for patient”, or “more time [is] spent on [EHR] than patient care.” Some of the other overall comments included “if I could I would exit this profession”, or “my belief is nothing will be done about the frustrations of staff.”
Conclusion(s): EHR implementation is initially associated with a significant increase in stress, with some improvement over time. Furthermore, qualitative responses note the considerable burden for charting and its perceived negative impact on patient care. The role of appropriate training and steps to increase buy-in from clinicians during a new implementation needs to be investigated.