Neonatology
Session: Neonatal Quality Improvement 2
394 - A QI Initiative to Optimize Attendance Rates at a NICU High Risk Follow-up Program
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 394
Publication Number: 394.1975
Publication Number: 394.1975
.jpg)
Tatiana A. Nuzum, MB BCh BAO (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Hassenfeld Children's Hospital at NYU Langone
New York, New York, United States
Presenting Author(s)
Background: NICU graduates are at risk for neurodevelopmental impairment (NDI), especially those born premature or with neurologic injuries. Our Neonatal Comprehensive Care Program (NCCP) is a high-risk neurodevelopmental follow-up clinic that performs developmental assessments until age 2. NCCP follows eligible graduates from two Level IV NICUs – NYU Langone and Bellevue Hospital (BH) Centers. BH serves a more diverse, socioeconomically disadvantaged population. Over 1-year, we noted that NCCP 1st-visit attendance rates for NYU infants was 70% but only 30% for BH infants. We also noticed that many BH infants with neurologic injury were never scheduled for NCCP.
Objective: To improve attendance rates of BH patients at 1st-visit appointments to 70% over one year.
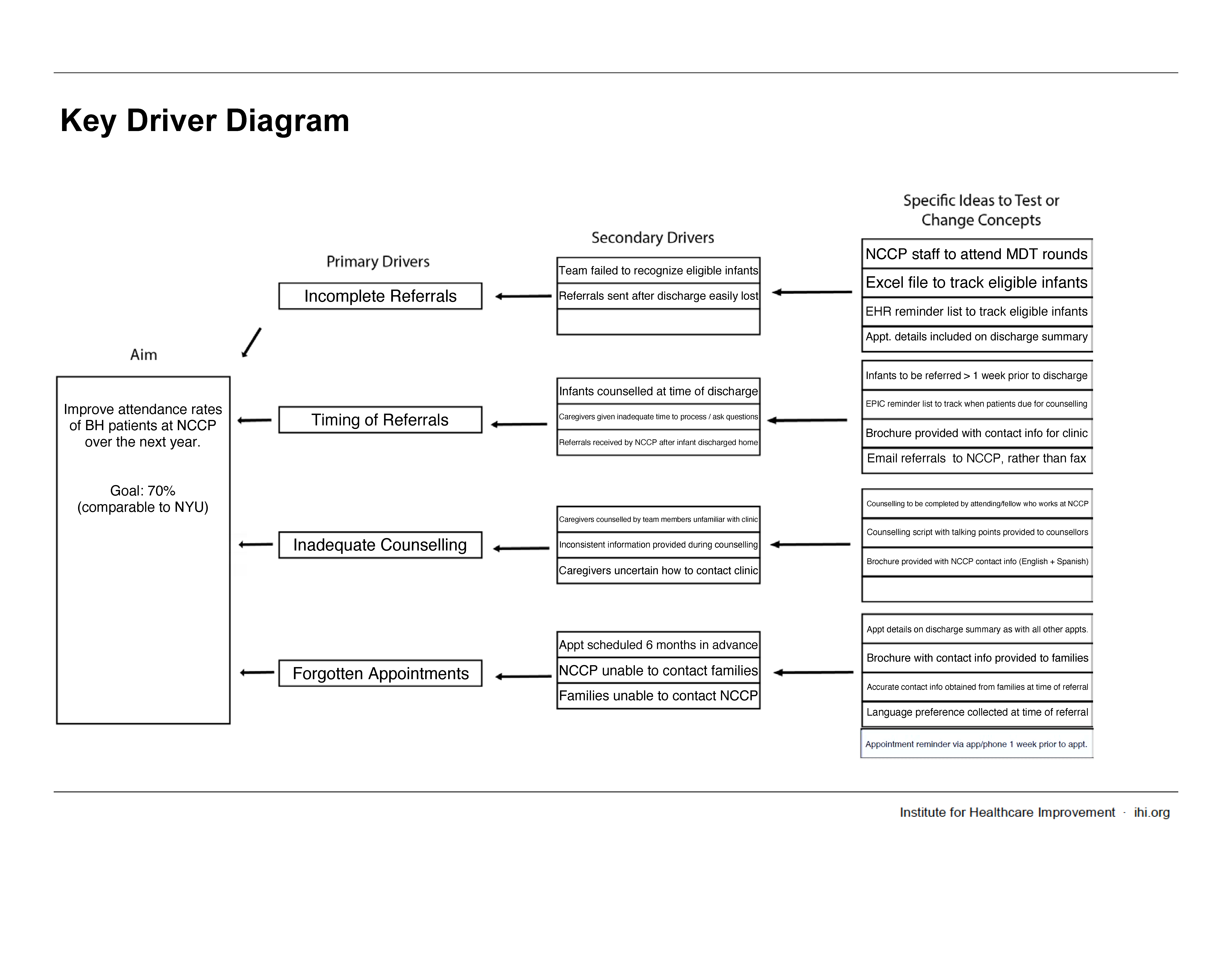
Design/Methods: Baseline attendance rates were collected from Oct 2021 to Sept 2022. A Key Driver Diagram (Figure 1) and Process Map was formulated to guide our approach which included a new scheduling process (PDSA #1) and counselling process (PDSA #2).
Scheduling process (PDSA #1 Oct 2022): The scheduling process was adjusted so that eligible infants were scheduled for an appointment prior to discharge and that information was included in the discharge summary. Online and EMR tracking systems were created to serve as reminders for when infants should be referred and scheduled. Accurate contact information and language of preference was obtained from caregivers prior to discharge, to allow for reminder calls one week prior to appointments.
Counseling process (PDSA #2 Apr 2023): The responsibility of counselling caregivers prior to discharge on the importance of NCCP was transferred to part of the medical team that was familiar with the clinic and had been provided education. A counselling script was created to ensure consistent, accurate information was provided. A clinic brochure, available in multiple languages, was also provided.
We followed attendance rates prospectively for 10 months to evaluate for change.
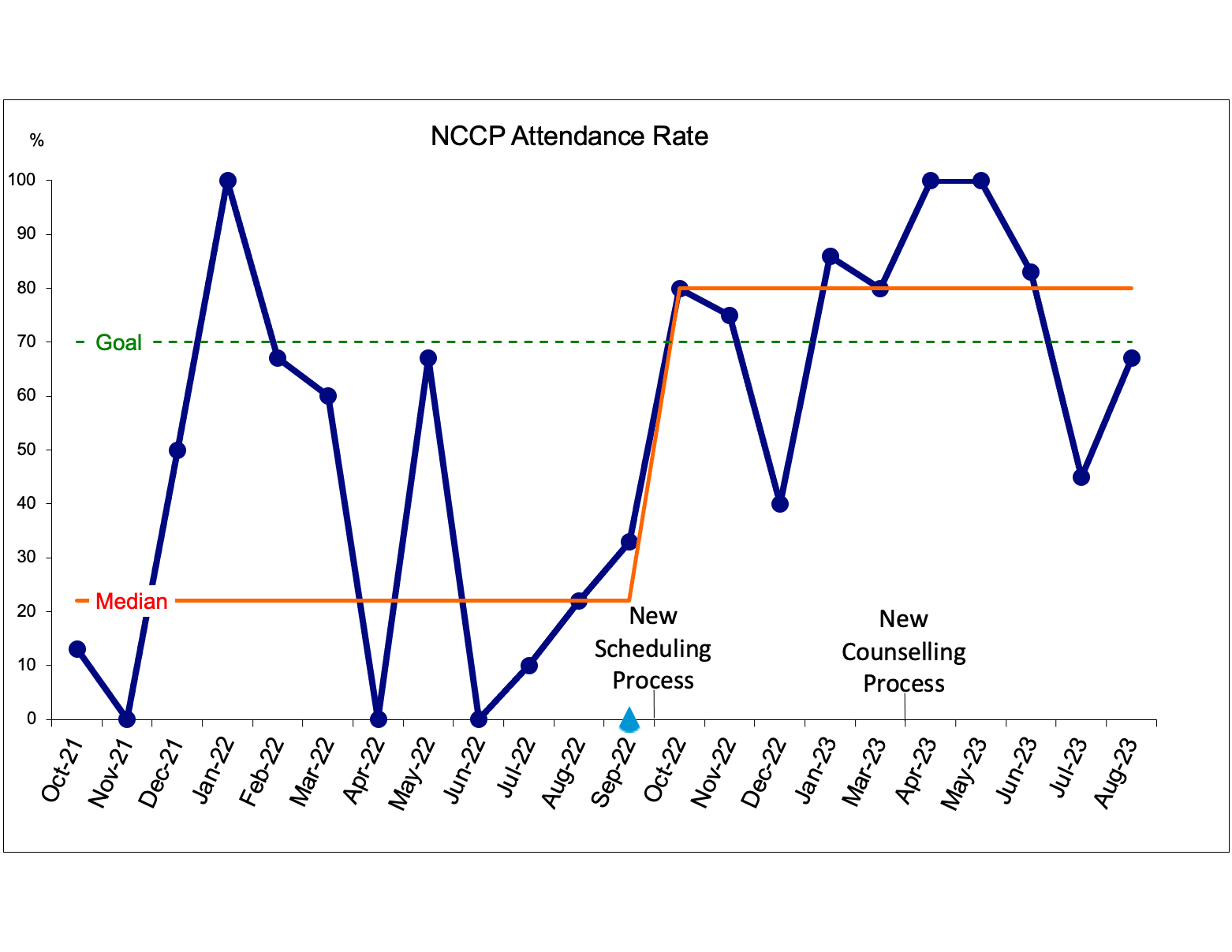
Results: Median attendance rates improved from 22% to 80% following interventions (Figure 2). Monthly attendance varied between 40-100%. Three to eleven infants were scheduled each month. No eligible infants were discharged home without being referred to NCCP.
Conclusion(s): A comprehensive scheduling and counselling process tailored to the needs of our population proved to be successful in improving NCCP attendance rates. Attendance rates exceeded our goal, which was set in an attempt to achieve equity between our clinic populations. Continuing to track attendance will determine long-term sustainability of these interventions.