Emergency Medicine
Session: Emergency Medicine 10: Trauma
393 - Barriers to Provider and Guardian Acceptance of Hematoma Blocks for Forearm Fracture Reductions in a Pediatric Emergency Department
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 393
Publication Number: 393.3041
Publication Number: 393.3041

Kristen C. Lau, PhD (she/her/hers)
Clinical Research Coordinator
Children's Hospital of Philadelphia
Philaldephia, Pennsylvania, United States
Presenting Author(s)
Background: Distal radius and/or ulna fractures commonly present in the pediatric emergency department (ED). Procedural sedation (PS) is the current preferred method of analgesia and anxiolysis to facilitate fracture reduction, but can be associated with adverse events, high resource utilization, and extended length of stay. Hematoma block (HB), often used with an anxiolytic agent, is an alternative, but underutilized option for fracture reduction. Reasons for lack of HB use in pediatrics is poorly understood.
Objective: To assess the willingness of pediatric emergency medicine (PEM) providers, orthopedic providers, and parents to consider HB as an alternative to PS for children requiring forearm fracture reduction in the pediatric ED.
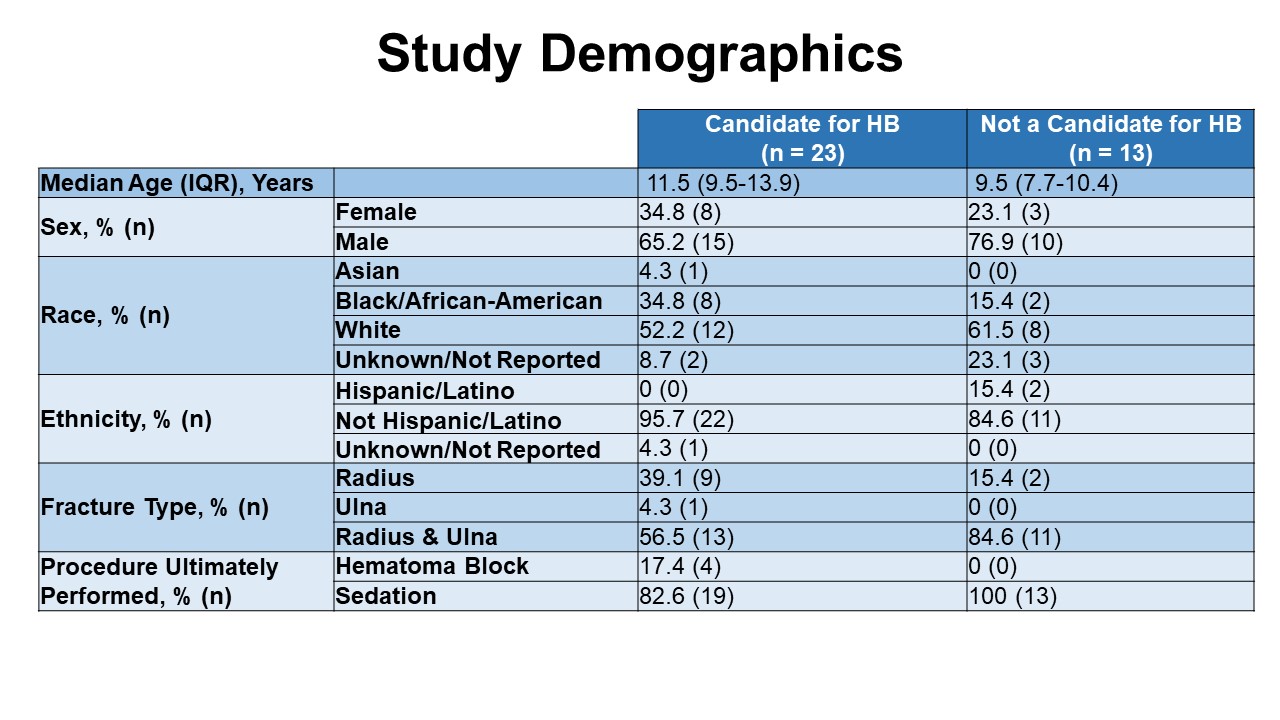
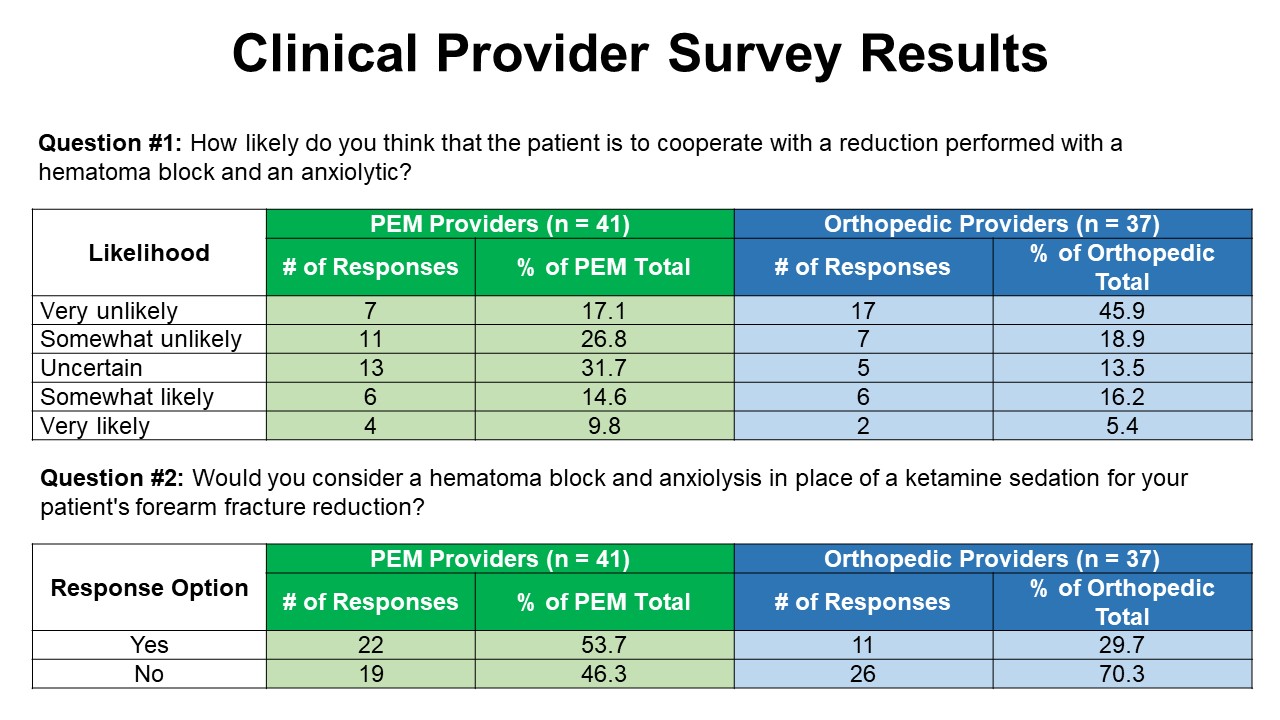
Design/Methods: We prospectively enrolled children aged 5-17 years from April-October 2023 with closed distal radius and/or ulna fractures requiring reduction in a single tertiary care children’s hospital. We excluded those with associated dislocations, additional fractures in the same extremity, and those requiring operative intervention. We surveyed PEM and orthopedic providers about qualifying patients during the ED visit to understand if they felt the child was a candidate for HB and to identify perceived barriers to HB performance. Parents were surveyed to assess willingness to learn about HB for fracture reduction.
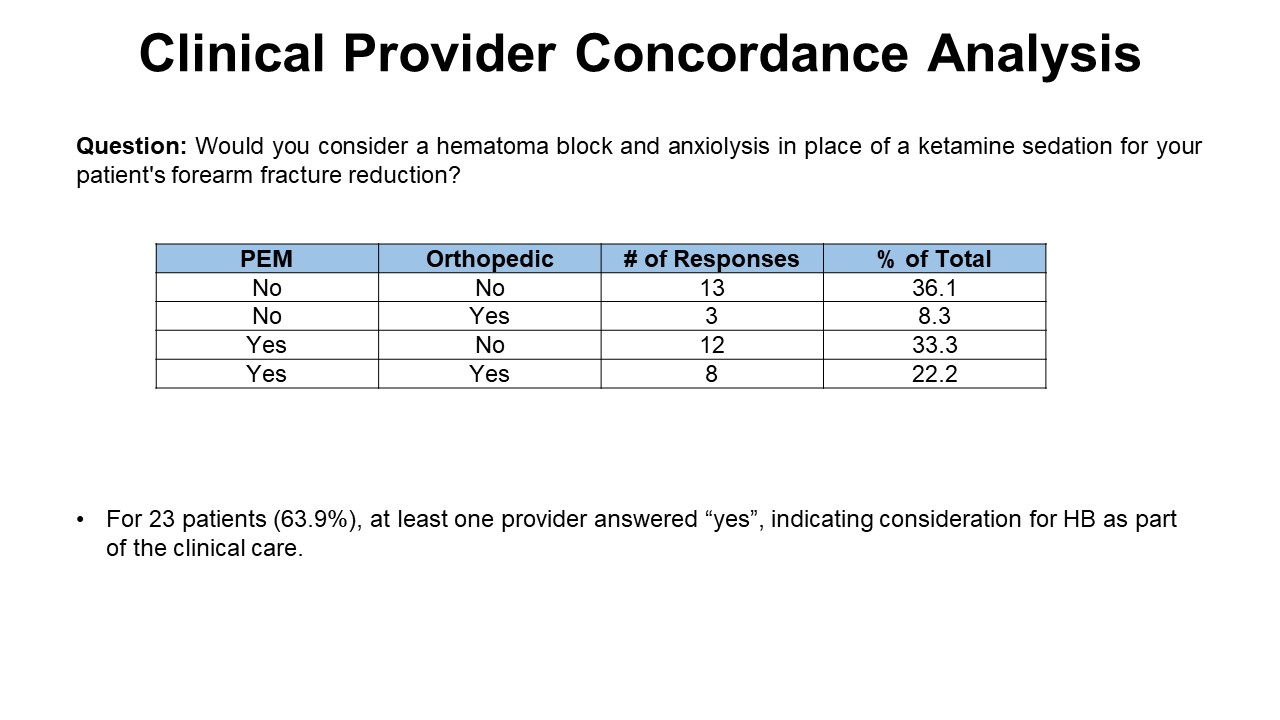
Results: Thirty-six patients were enrolled with fully completed provider surveys. Orthopedic providers were willing to offer HB in 30.6% of subjects and PEM providers were willing to offer HB in 55.6%. Concordance between provider response was assessed. For 13 subjects (36.1%), providers agreed HB was not suitable for forearm reduction. For 8 subjects (22.2%), providers agreed HB was a suitable option.
At least one of the providers was willing to consider HB in 23 patients (64%). Patients suitable for HB had a median age of 11.5 years; those considered unsuitable had a median age of 9.5 years. Fifty-percent of those suitable for HB received HB as part of their treatment.
Parents of 35 subjects completed surveys: 60% expressed interest in learning about HB as an alternative to PS.
Conclusion(s): HB is likely an underutilized means of fracture reduction in pediatrics, but this study shows that in over half of the patients, as least one of the providers was willing to consider HB. Preliminary results indicate that age was a common consideration when determining if a patient was a good candidate for HB. This study underscores the need to further investigate the ideal characteristics of patients likely to successfully undergo HB.