Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 4
16 - A Quality Improvement Project to Support Implementation of the New Pediatric Obesity Guideline During Well Visits
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 16
Publication Number: 16.3042
Publication Number: 16.3042

Janice Liebhart, MS (she/her/hers)
Evaluation Manager
American Academy of Pediatrics
Itasca, Illinois, United States
Presenting Author(s)
Background: In January 2023, the American Academy of Pediatrics published the Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents With Obesity (CPG). A 25-week, virtual, team-based quality improvement (QI) collaborative was launched in March 2023 to support CPG implementation during well visits.
Objective: To examine results-to-date for clinical measures during the pilot.
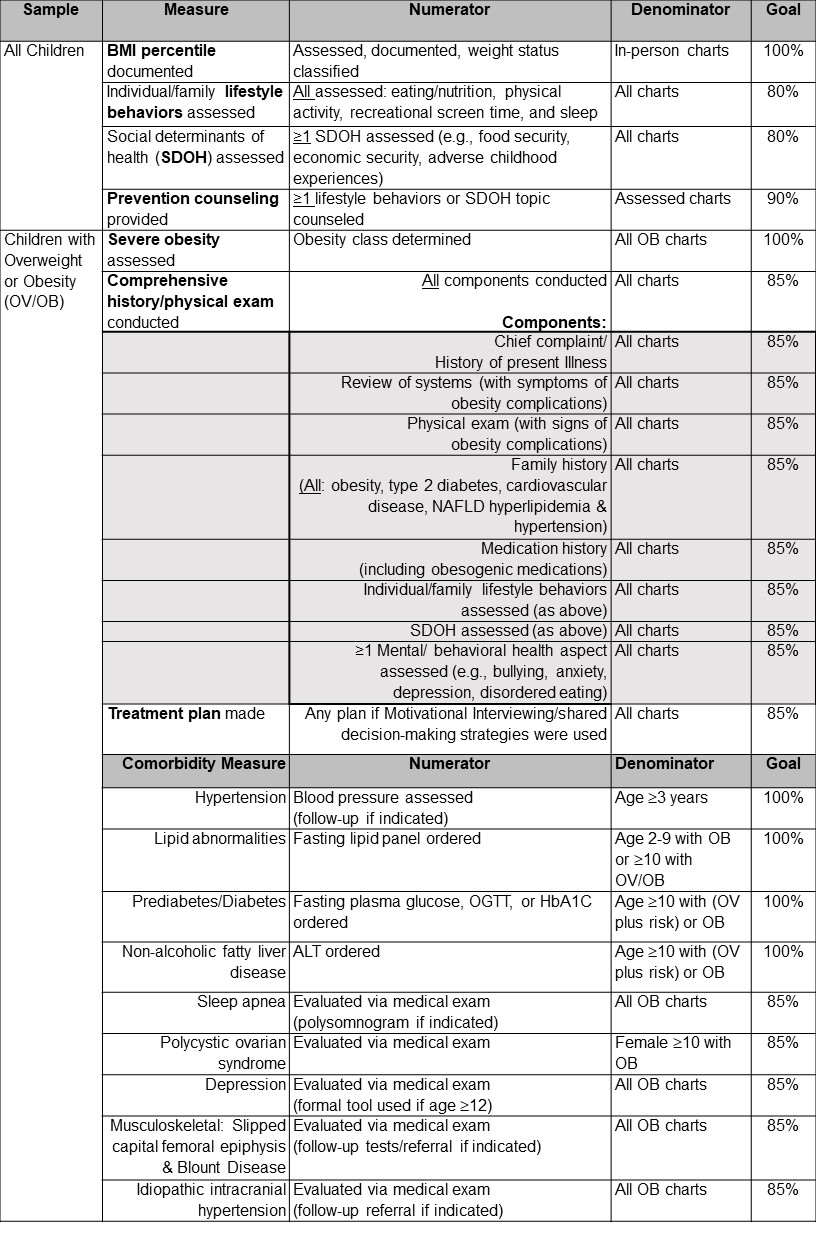
Design/Methods: 15 teams from diverse practice sites are participating (e.g., 9 US states; 6/15 Federally Qualified Health Centers), with a potential reach of >300 providers and >110,000 pediatric patients. Teams complete online trainings, conduct local meetings and Plan-Do-Study-Act cycles, and attend national webinars. Provided resources include a Key Driver Diagram & change package with various new tools/resources. Teams submit 3 cycles of clinical data during the collaborative and 1 monitoring data cycle 4 months later. For each cycle, teams submit randomly selected charts from 2 well visit samples: all children ages 2-18 (10 charts) & children with overweight/obesity (OV/OB) (20 charts). 4 measures for all children include 3 assessments--BMI percentile, Lifestyle behaviors, Social determinants of health (SDOH)--and Prevention counseling (Table). 12 measures for children with OV/OB include Severe obesity assessment, Comprehensive history/physical exam (8 required subcomponents), shared Treatment plan, and 9 Comorbidity evaluation measures: Hypertension, Lipids, Diabetes, Non-alcoholic fatty liver disease (NAFLD), Sleep Apnea, Polycystic ovarian syndrome (PCOS), Depression, Slipped capital femoral epiphysis (SCFE)/Blount Disease, & Idiopathic intracranial hypertension (IIH). Comparisons of aggregate clinical measures at baseline versus at cycles 2 and 3 are based on Fisher’s Exact Test at p<.025 (2 comparisons).
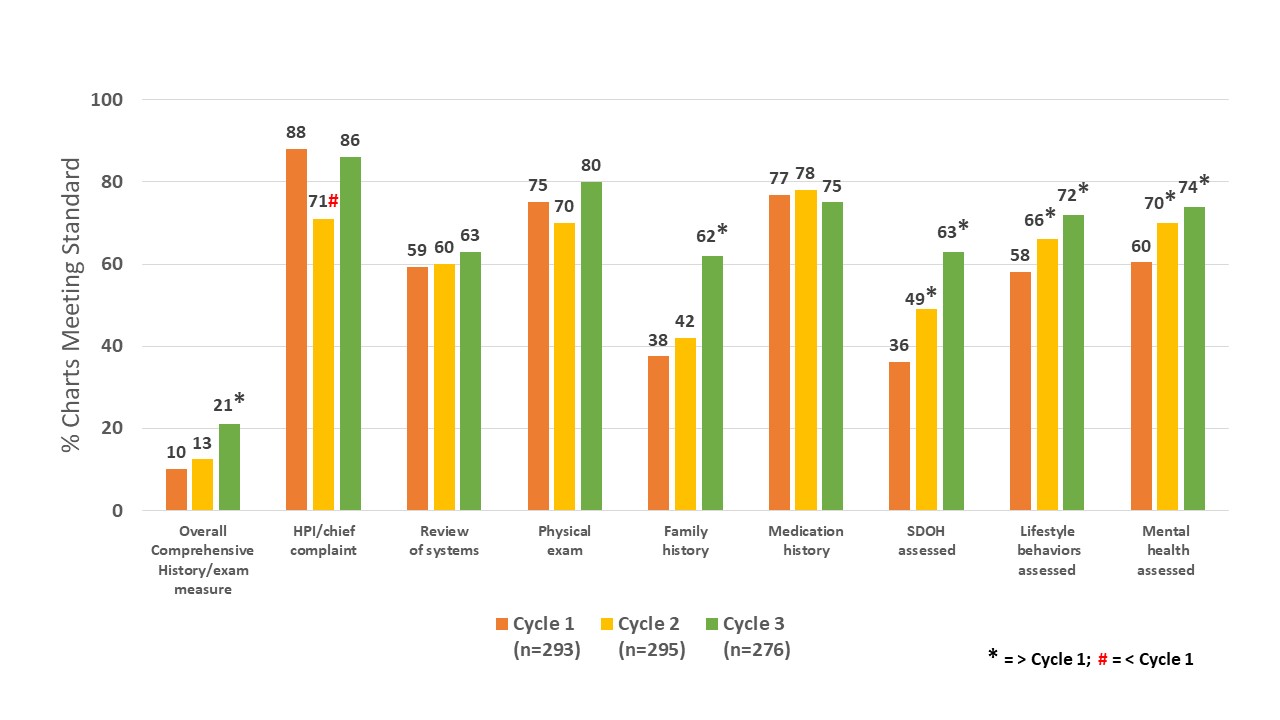
Results: Baseline values supported a need for improvement, relative to new CPG standards. By cycle 3, significant increases were observed for 4/4 measures for all children and 9/12 measures for children with OV/OB (Figure 1). Improvements were most notable for several relatively low measures at baseline, but room for improvement typically remained. Half of the subcomponents of a comprehensive history/physical exam also improved, although the overall measure remained low (Figure 2).
Conclusion(s): Primary care teams participating in a brief QI collaborative to improve well visit care relative to 2023 standards improved all universal measures and 75% of measures for children with OV/OB. Limitations include a small number of teams and a pending monitoring data cycle, but potential reach is substantial.