Neonatology
Session: Neonatal Quality Improvement 2
407 - Sustaining Unplanned Extubation Reduction in the NICU: A Collaborative Approach Using Shared Mental Models
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 407
Publication Number: 407.1988
Publication Number: 407.1988
- MS
Meenakshi Singh, MBBS (she/her/hers)
NICU Director of Quality
Maria Fareri Children's Hospital at Westchester Medical Center
Valhalla, New York, United States
Presenting Author(s)
Background: Unplanned extubation (UE) in the Neonatal Intensive Care Unit (NICU) is a matter of substantial safety hazard and is increasingly recognized as an important quality indicator of patient safety in the NICU. Complications of UE include acute cardiorespiratory events, complications related to bag and mask ventilation, and risks of injury related to repeated intubations .Quality improvement (QI) studies have indicated that using a multi-prong approach has been successful in reducing rates of UE in neonates . Implementing a systematic approach to reduce UE in a large busy unit with no preexisting formal system of audits or structure remains a challenge. Central to our study's novelty is the integration of the shared mental model approach which stands as a cornerstone, guiding our efforts to address challenges and foster collaborative problem-solving .
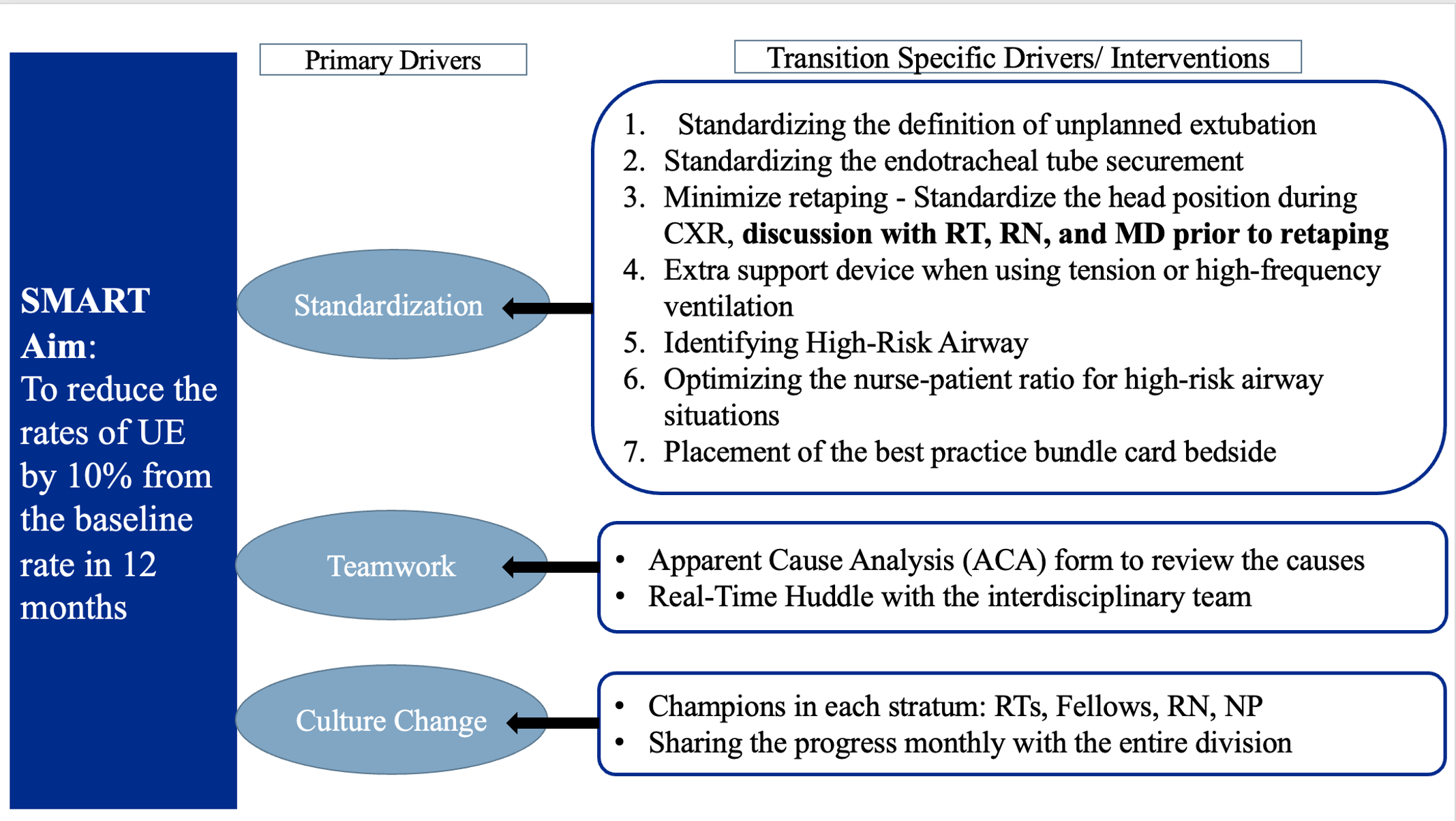
Objective: SMART
Aim: To decrease the rate of UE by 10% from the baseline in 12 months.
Design/Methods: All UE were identified using a data collection tool, the Apparent Cause Analysis (ACA) form. ACA form was used to identify the causes related to UE and key areas for improvement. Interventions were implemented in a step-by-step fashion and reviewed monthly using the model for improvement. (Figure 1)
The concept of best practice huddles and shared mental models were introduced. Interventions were focused to promote a cultural change that emphasizes the importance of standardization measures and shared decision-making
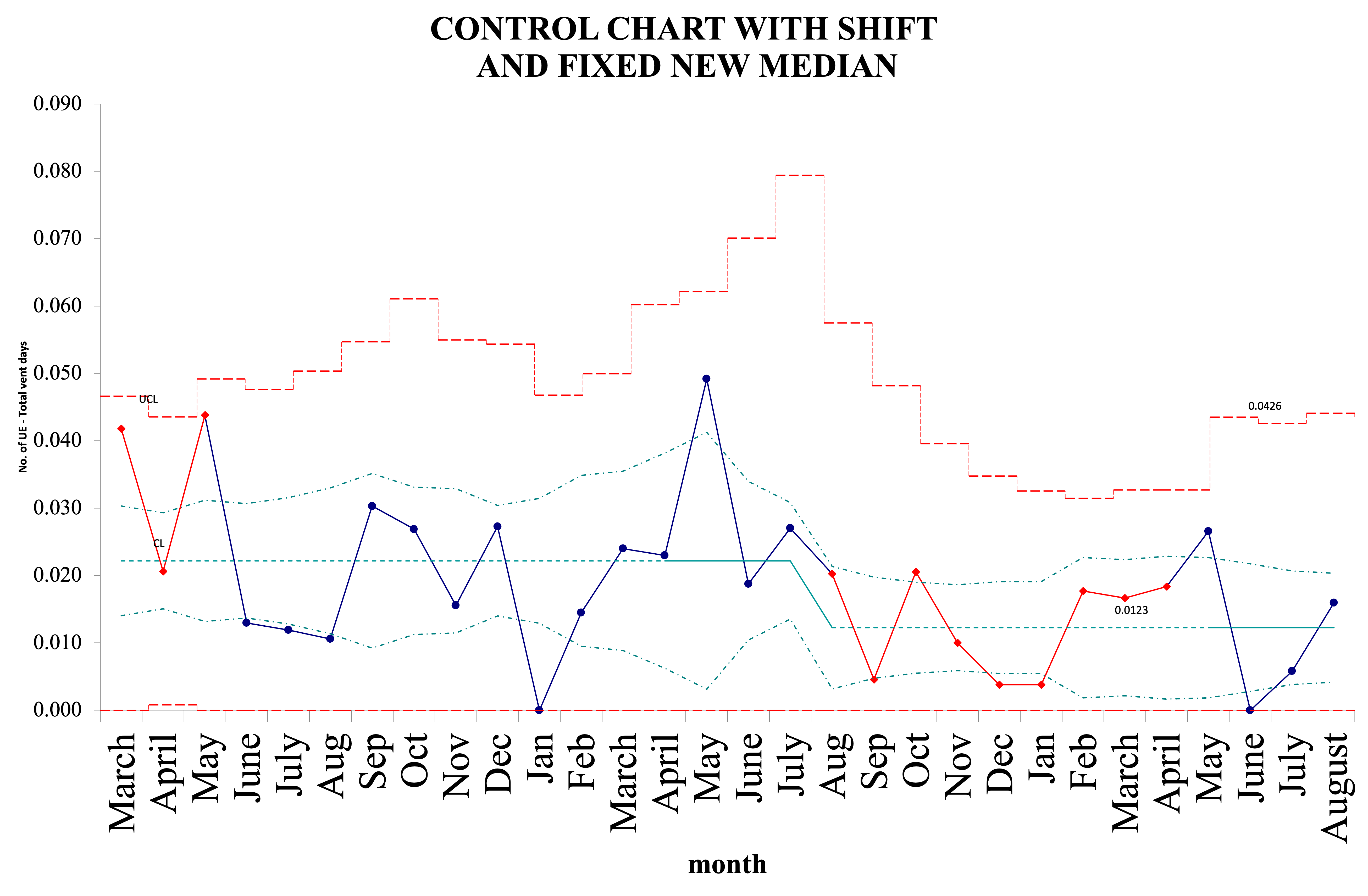
Results: The baseline UE rate was 2.3/100 ventilator days. Retaping, bedside care, and position change accounted for over 50% of the UE events in 2022. 86% of the events required reintubation. From August 2022, the rates remained below the median of 2.3 per 100 ventilator days for more than 8 consecutive months. We achieved a sustained shift in the median and the new median was fixed at 1.1/100 ventilator days. (Figure 2)
Conclusion(s): This QI initiative provides a roadmap to address a deep-rooted multifactorial problem in the NICU with a well-organized and phased quality improvement tool. It underlines the importance of shared decision-making to tackle long-standing system problems and improve outcomes. We suggest a model of shared decision-making between the RT, nurse, and medical provider to discuss the ETT position on imaging in regard to head positioning, tension applied, and the clinical status of the infant. To sustain the improvement, we emphasize the necessity of instilling a culture change, wherein UE is recognized as a "never event" in the NICU