Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 4
20 - CT Scan Utilization Decreases with Implementation of an Imaging Pathway for Children with Suspected Acute Appendicitis
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 20
Publication Number: 20.3025
Publication Number: 20.3025

Julia N. Lo Cascio, B.S.
Medical Student
New York University Long Island School of Medicine
Staten Island, NY, New York, United States
Presenting Author(s)
Background: In the United States, approximately 70,000 children are diagnosed with appendicitis each year [1]. Computed tomography (CT) is increasingly utilized in emergency room settings, due to its high sensitivity and specificity, as well as the ability to rule out a multitude of alternative diagnoses [2]. However, pediatric patients are particularly susceptible to the ionizing radiation exposure with estimates that the life-time risk of pediatric CT-associated leukemia is 1-in-7500, and brain cancer is 1-in-1000 [3]. CT should therefore only be used when non-radiating alternatives, such as magnetic resonance imaging (MRI) and ultrasonography (US), are unavailable or inconclusive [4]. This has led to children’s hospitals participating in the National Surgical Quality Improvement Program-Pediatric (NSQIP-P) to reduce CT scan use to 25% in children with suspected appendicitis [5].
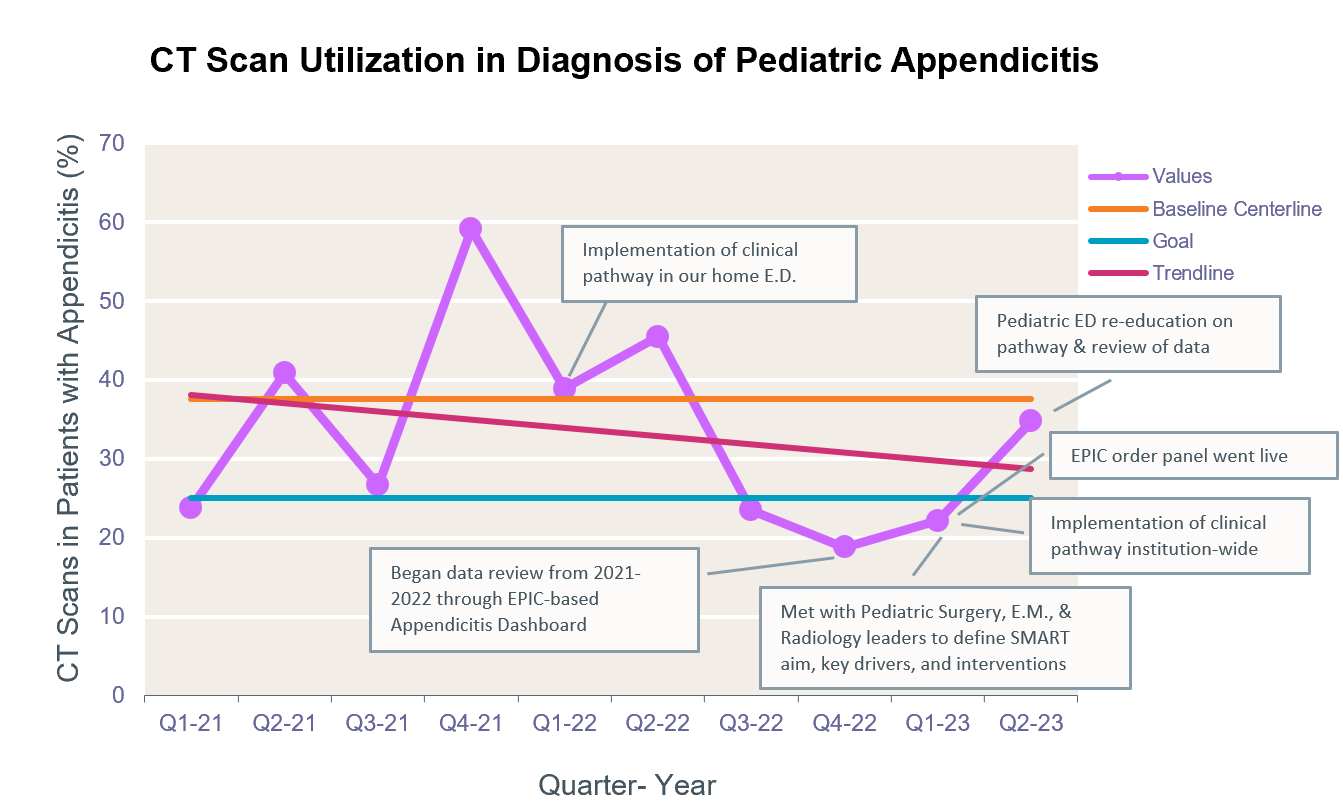
Objective: In 2022, a multidisciplinary team at our institution mapped the current process in pediatric appendicitis evaluation and management to define improvement opportunities and outlined key drivers.
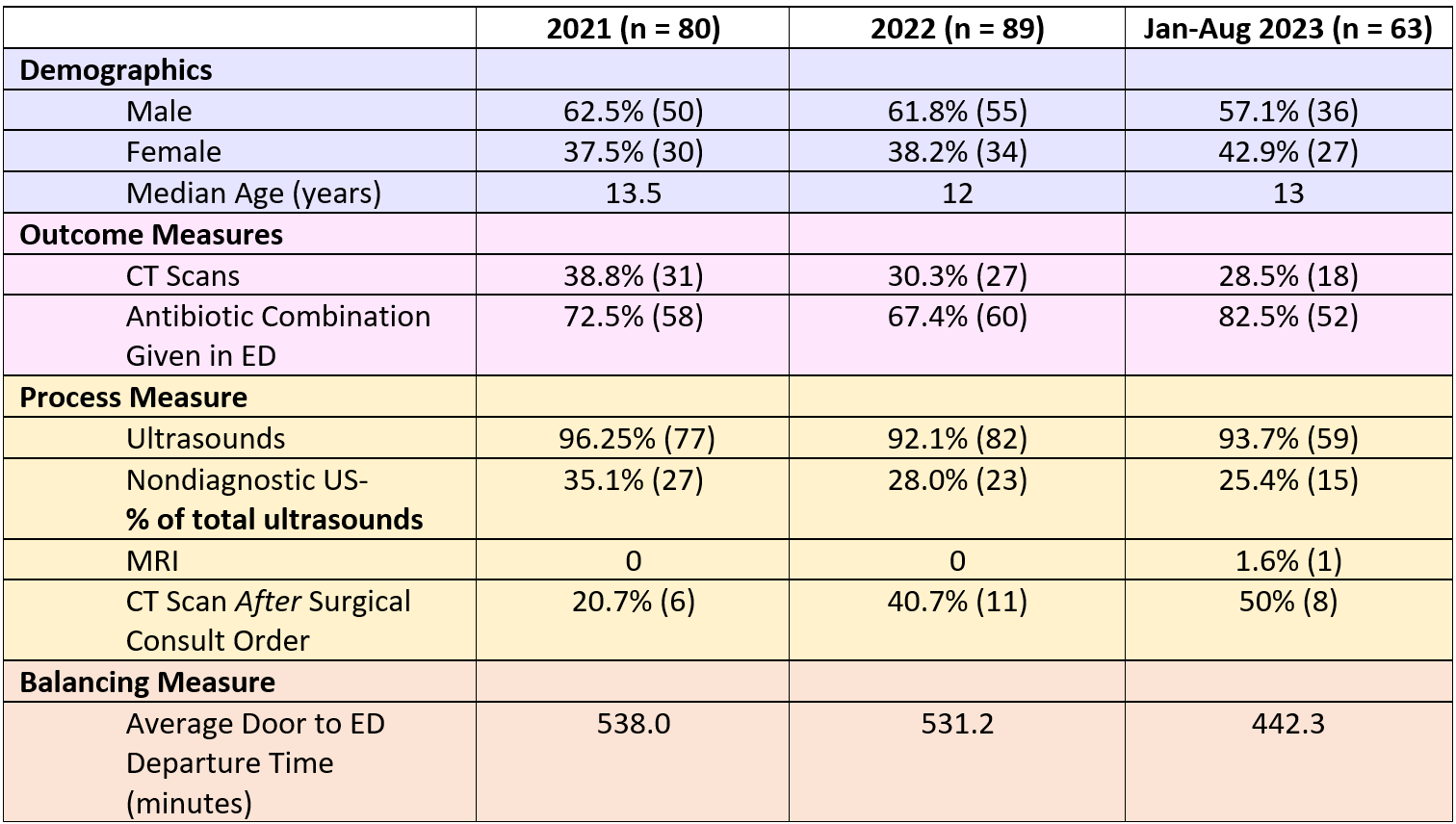
Design/Methods: The main key driver was the development of a Pediatric Appendicitis Clinical Pathway and our intervention was carried out in a series of PDSA cycles. This pathway emphasizes the use of US as first-line imaging in patients with suspected appendicitis and reserves CT for patients with both non diagnostic ultrasounds and agreement from pediatric emergency medicine and surgery that CT is appropriate. MRI is an alternative to CT, however, due to limited MRI resources at our institution, MRI is unlikely to occur in a timely fashion.We reviewed all cases of patients ages less than 19 years old who were diagnosed with acute appendicitis from January 2021-August 2023, with data from 2021 serving as baseline data.
Results: We found that for all three years, ultrasound was the first line imaging in over 90% of cases. However, CT utilization after non diagnostic ultrasounds steadily decreased between 2021, 2022, and 2023 from 36% to 30% to 29%, respectively. This was paralleled by a sharp increase in surgical consults prior to CT scan order from 21% to 41% to 50%, respectively, as well as a decrease in non-diagnostic ultrasounds from 36% of total ultrasounds to 28% to 26%, respectively.As a balancing measure, we monitored time spent in the ED, which decreased from 538 minutes in 2021 to 531 minutes in 2022 to 442 minutes in 2023, on average.
Conclusion(s): Overall, by implementing a Pediatric Appendicitis Clinical Pathway, we were able to reduce CT scan utilization in the diagnosis of pediatric appendicitis.
.png)