Neonatology
Session: Neonatal Quality Improvement 4
66 - Preventing Neonatal Hypothermia in the Delivery Room: A Quality Improvement Initiative for Moderate- and Late-Preterm Infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 66
Publication Number: 66.3023
Publication Number: 66.3023

Amanda E. Winkler, MD (she/her/hers)
Fellow
Boston Children's Hospital
Belmont, Massachusetts, United States
Presenting Author(s)
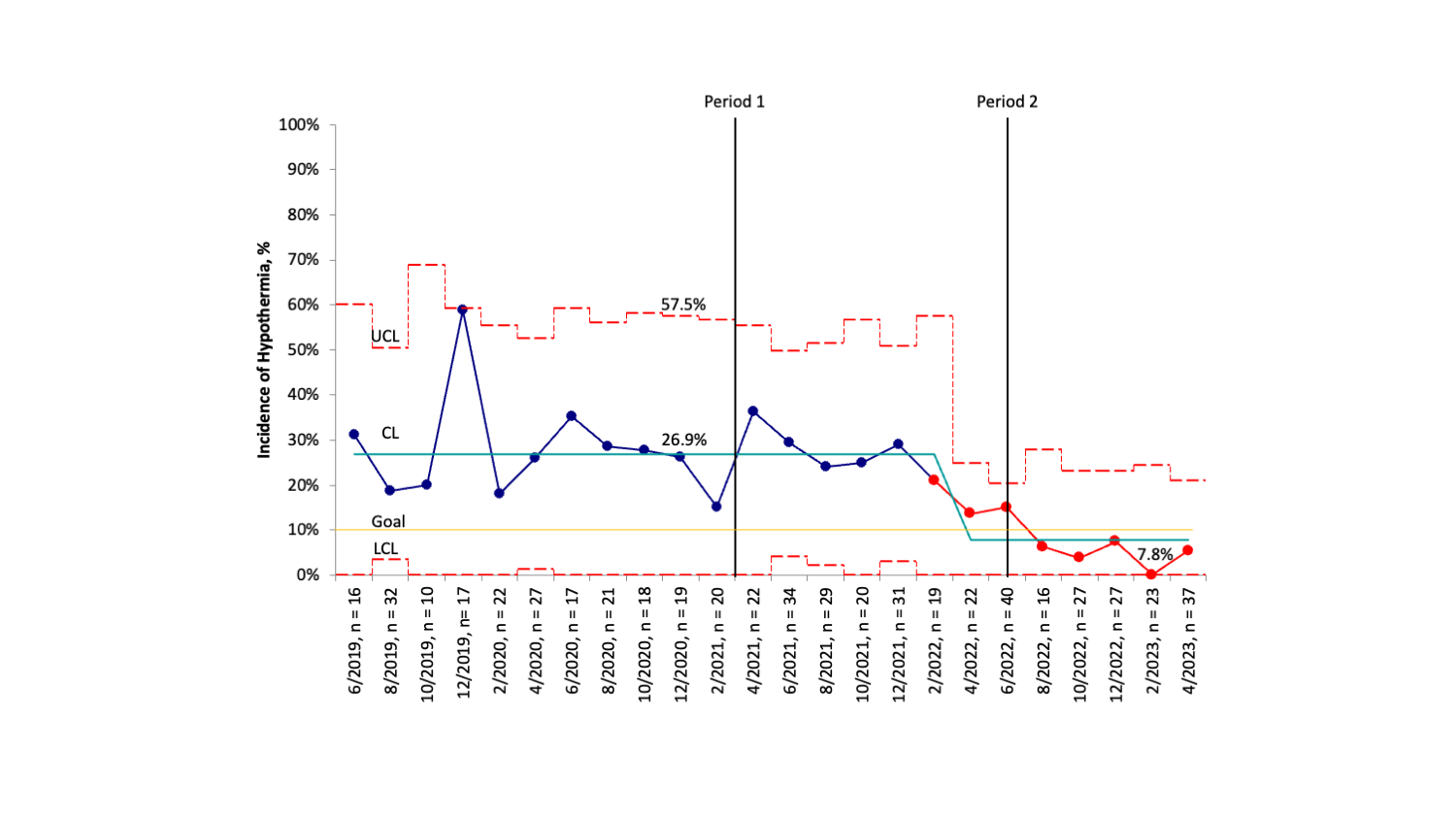
Background: Neonatal hypothermia is a common and preventable cause of neonatal morbidity and mortality. While the prevention of hypothermia has been extensively studied in infants < 32 weeks gestation, few studies have evaluated hypothermia prevention targeting moderate- and late-preterm infants (MLPI) in the delivery room. At our institution, approximately 26% of MLPI developed hypothermia, defined as a temperature < 36.5 C per World Health Organization guidelines, at the time of neonatal intensive care unit (NICU) admission. In comparison to infants < 32 weeks gestation, MLPI were 63% more likely to meet criteria for hypothermia.
Objective: The aim of this study was to expand the use of thermoregulation techniques used in infants < 32 weeks gestation to MLPI to decrease the rate of NICU admission hypothermia from 26% to less than 10% over a period of two years.
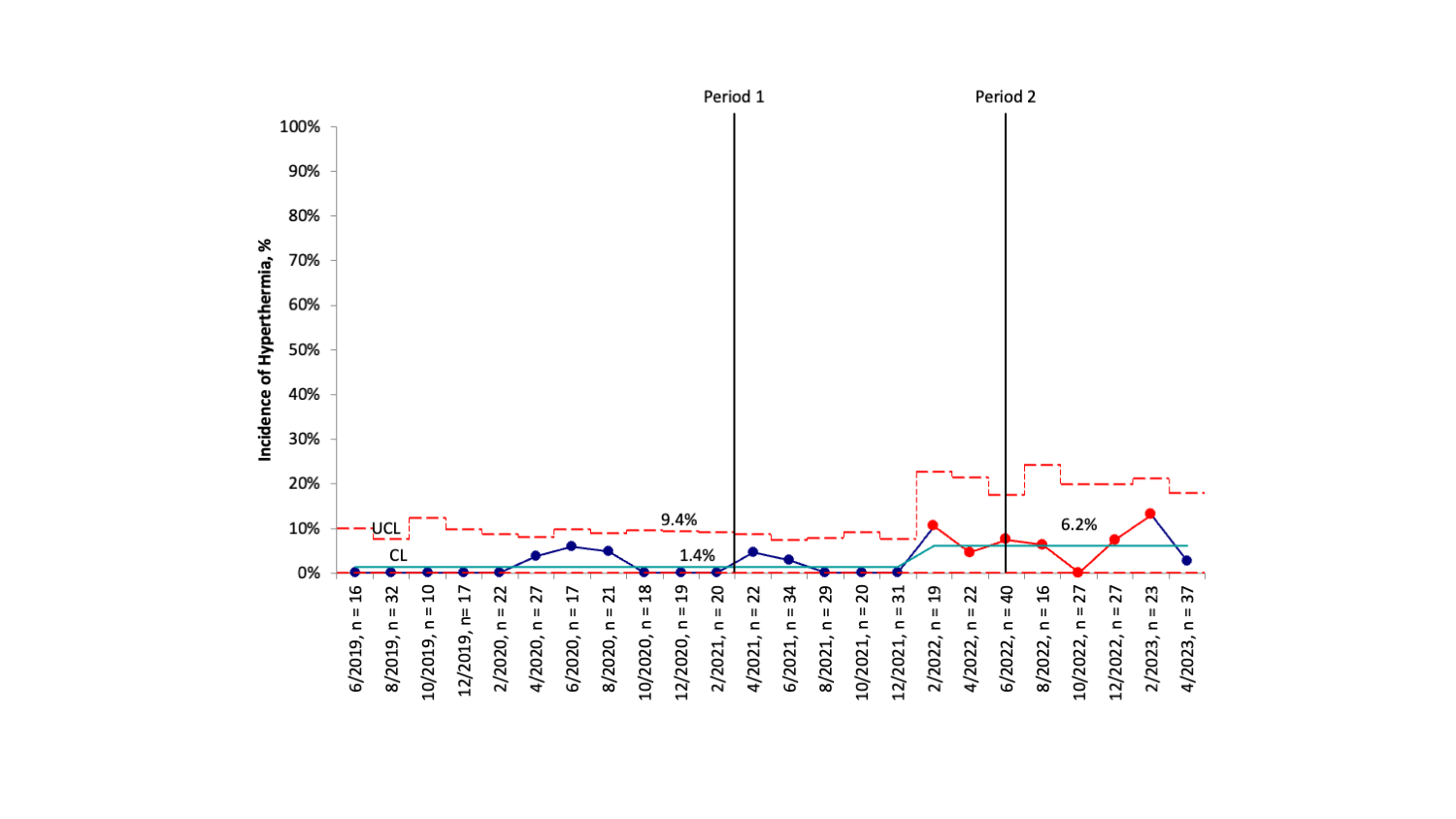
Design/Methods: This quality improvement initiative was conducted from June 2019 to June 2023 in a level IV NICU and Labor and Delivery Unit of a large academic hospital. All inborn MLPI, 32 + 0/7 to 36 + 6/7 weeks gestation, admitted to the NICU were included. To this population, we expanded thermoregulatory measures typically used in bundles for infants < 32 weeks gestation including increased delivery room ambient temperature to 74 F (Period 1) and thermal mattress use (Period 2). The primary outcome was hypothermia ( < 36.5 C) upon NICU admission. The balancing measure was hyperthermia (>/= 38 C).
Results: During the study period, there were 566 inborn MLPI with a mean gestational age of 34 + 3/7 weeks and a mean birth weight of 2269 g. Special cause variation in the incidence of neonatal hypothermia was observed. The incidence of hypothermia was reduced 71% from a mean baseline of 26.9% to 7.8% post-intervention. Special cause variation was also observed in the incidence of hyperthermia with an increase from 1.4% to 6.2% with all but one case 99 F. All cases of hyperthermia resolved within two hours of NICU admission.
Conclusion(s): Expansion of several thermoregulation techniques commonly used in infants < 32 weeks gestation, particularly thermal mattress use, was associated with decreased incidence of NICU admission hypothermia in MLPI with an associated increase in mild hyperthermia. When using the thermal mattress in the MLPI population, temperatures should be monitored closely, and the thermal mattress removed, if patient temperature trends outside of acceptable parameters.